Behind the Research: Sex and Gender Medicine in Physician Training, a 10-Year Follow-Up at Cedars-Sinai
Published in Education
Why this study was necessary
In 2014, we surveyed physician trainees at Cedars-Sinai to assess how often topics related to sex (biological differences) and gender (socially constructed roles) were addressed in their clinical and didactic education. Despite growing awareness of sex and gender differences in disease patterns and treatment response, we found that most trainees reported little to no exposure.
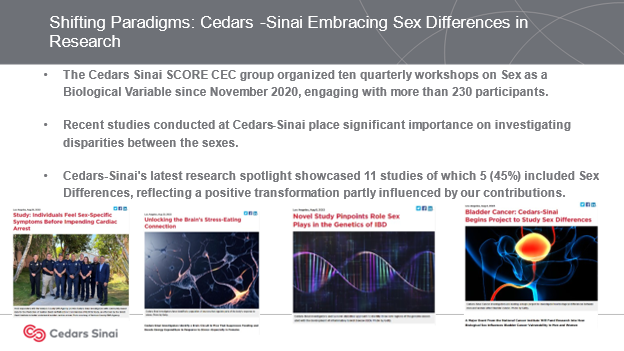
In the years since, our institution made concerted efforts to bridge this gap. With support from the NIH-sponsored Specialized Center of Research Excellence (SCORE) and our Center for Excellence in Sex Differences in Medicine (CEC), Cedars-Sinai introduced new requirements for grand rounds, embedded sex-based decision tools in clinical practice, and launched educational workshops. A decade later, we wanted to evaluate whether these efforts had increased awareness and exposure in physician training.
What we did
In February 2024, we repeated the original survey with current residents and fellows at Cedars-Sinai. The instrument was nearly identical to the 2014 version, allowing us to directly compare trainee attitudes and perceived exposure over time.
We distributed the anonymous survey to 490 postgraduate trainees and received 62 responses, similar to the participation level in 2014.
What we found
While enthusiasm for sex and gender medicine remained strong, perceived exposure had changed little since 2014.
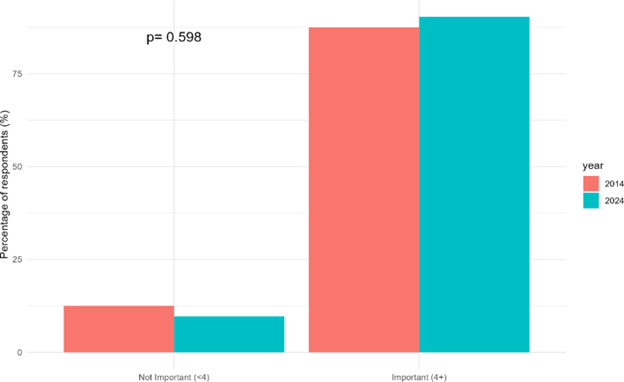
- 90% of respondents in 2024 said sex and gender medicine is important, virtually identical to the 88% from 2014.
- 53% supported a formal curriculum, comparable to 60% in 2014.
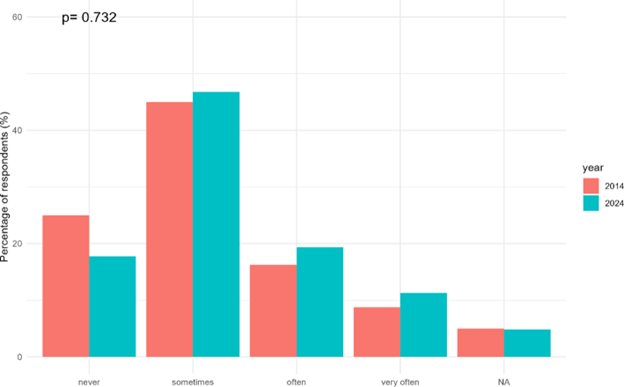
- Only 31% reported hearing about sex and gender concepts "often" or "very often" in clinical teaching, versus 25% in 2014.
- 95% said they incorporate sex into patient care.
- 82% believed additional training would help reduce bias and improve care.
These results suggest that while trainees recognize the importance of sex and gender in medicine, this content is still not consistently taught in clinical settings.
Institutional efforts and persistent challenges
Over the past ten years, Cedars-Sinai implemented several initiatives to advance sex and gender awareness in clinical education:
- Required all CME speakers to address sex as a biological variable
- Developed tools to integrate sex-based differences into diagnostic pathways
- Offered SCORE-supported workshops and mentorship for trainees
- Embedded sex and gender topics into select lectures and research projects
Despite these efforts, trainees still reported rare inclusion of sex and gender in their daily clinical learning. This suggests that occasional top-down interventions may be insufficient unless these concepts are routinely reinforced at the point of care by attending physicians and supervisors.
Reflections from the research team
One surprising and encouraging result was the continued increase in support from male trainees, whose endorsement of sex and gender medicine now closely matches that of female peers. This shift reflects broader cultural progress in medical education and highlights the universal relevance of these concepts to patient care.
Still, the dissonance remains: most trainees say sex and gender matter, but few report frequent exposure during their training. This gap between recognition and education underscores the need to make sex and gender medicine a consistent part of graduate medical education.
What this means for the future of medical training
To close this gap, we recommend a multi-pronged strategy:
- Integrate sex and gender content across all specialties, not just as optional lectures
- Provide structured training for faculty to help them incorporate these topics into everyday teaching
- Include sex and gender medicine as required competencies for board certification
- Develop and share clinical decision tools that normalize SABV (sex as a biological variable) in care delivery
Although this study was conducted at a single site with a modest response rate, it reinforces national findings that change has been slow. The consistent trainee support shows there is a clear appetite for better education.
Looking ahead
From our earliest survey in 2014 to this follow-up in 2024, the story has remained remarkably consistent: trainees care about sex and gender medicine and want more education, but they are not consistently receiving it. This study helped clarify how institutional efforts have helped—and where they fall short.
Our hope is that this research sparks renewed attention to how clinical training can better reflect what we know about biological and gender-related differences. We invite other institutions to replicate similar surveys and share their findings so we can accelerate progress together.
Follow the Topic
-
Discover Medicine

This is a fully open access, peer-reviewed journal that supports multidisciplinary research and policy developments across the fields of medical and clinical science.
Related Collections
With Collections, you can get published faster and increase your visibility.
Gender and Ethnic Disparities in Cardiovascular Health and Diseases
The global burden of cardiovascular disease (CVD) is alarming, with profound gender and ethnic disparities. Women are more likely to be underdiagnosed and undertreated, while ethnic minorities, including African Americans, Hispanics/Latinos, American Indians, and those in underserved communities, bear a disproportionate burden of CVD. Socioeconomic factors, inadequate healthcare access, and cultural barriers exacerbate these disparities. These disparities are not only a reflection of biological differences but also encompass a complex interplay of social determinants, healthcare access, and cultural factors. Understanding these dimensions is crucial for developing effective prevention and intervention strategies aimed at mitigating cardiovascular health inequalities. To bridge these gaps, rigorous research, robust data collection, and effective dissemination of findings are imperative in identifying these drivers.
This Collection will provide a platform for experts to share their research, insights, and solutions to address these pressing issues. We believe this Collection will contribute significantly to the ongoing conversation on health disparities and inform strategies to reduce the burden of CVD. We invite researchers and scientists to submit their original work to our Collection focused on gender and ethnic disparities in cardiovascular health and diseases. This Collection will contribute significantly to our understanding of the complex relationships between gender, ethnicity, and cardiovascular health outcomes and provide valuable insights into the drivers of these disparities and inform strategies for improvement.
Topics of interest include, but are not limited to:
- Gender differences in cardiovascular disease prevalence
- Ethnic disparities in treatment outcomes
- Sociocultural influences on cardiovascular health
- Impact of social determinants on heart disease risk
- Community-based interventions for at-risk populations
Keywords: Cardiovascular Disease Disparities, Gender and Ethnic Disparities in Health, Healthcare Access and Outcomes, Cardiovascular Health Equity, Racial and Ethnic Disparities in Cardiovascular Disease
This Collection supports and amplifies research related to SDG 3.
Publishing Model: Open Access
Deadline: Apr 14, 2026
Innovative Laboratory and Epidemiological Strategies to Reduce Mortality of Non-Communicable Chronic Diseases
Non-communicable chronic diseases (NCDs) and related conditions remain the leading causes of morbidity and mortality worldwide. These include two major categories: non-communicable chronic diseases—such as cardiovascular diseases, chronic respiratory diseases, and diabetes mellitus—and external causes, including accidents and violence. In parallel, advances in laboratory sciences and the growing field of precision medicine have opened new possibilities for early diagnosis, risk stratification, and personalized management. These approaches aim not only to identify individuals at greater risk of developing NCDs, but also to monitor disease progression and the emergence of complications or comorbidities. In this context, innovative laboratory methods and novel biomarkers are urgently needed to enhance disease detection and surveillance strategies. We therefore invite researchers to submit original articles, reviews, and case studies addressing the role of precision medicine in improving the surveillance and clinical management of chronic non-communicable diseases and their progression.
Keywords: Non-communicable chronic diseases; disease aggravation; biomarkers; laboratory methods; epidemiological aspects; individual risk classification; precision medicine; health promotion; surveillance; innovative laboratory approaches.
Publishing Model: Open Access
Deadline: Mar 23, 2026


Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in