Modular Endoprosthesis vs. Cement Spacer After Proximal Humerus Tumor Resection — Do We Really Gain Functional Advantage?
Published in Surgery
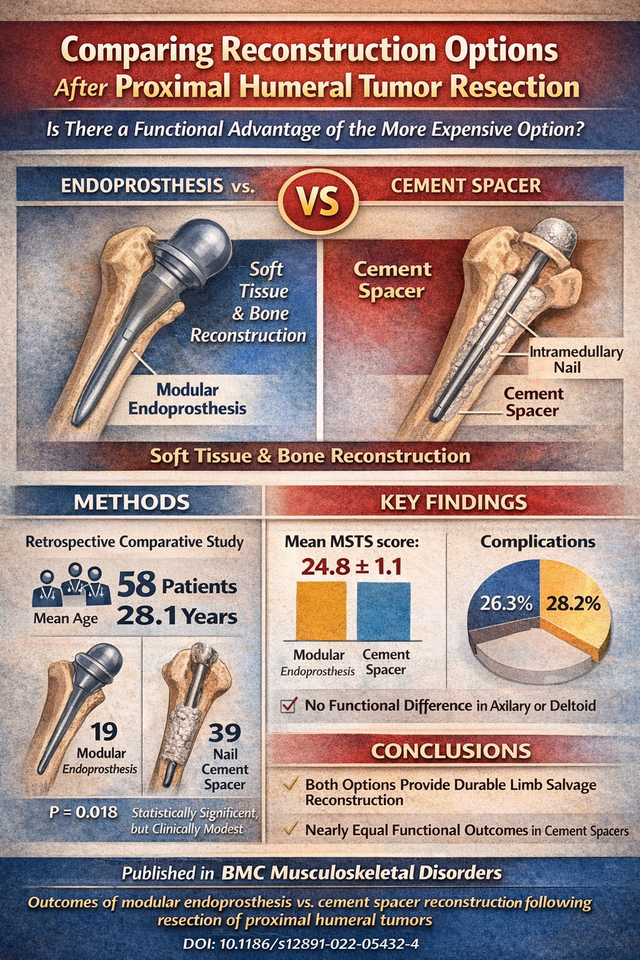
Reconstruction following wide resection of proximal humeral tumors remains controversial. While modular endoprostheses are often considered the more “advanced” option, their cost and potential complications raise an important question:
Do they truly provide superior functional outcomes compared to cement spacers?
In our retrospective comparative study published in BMC Musculoskeletal Disorders, we evaluated outcomes in 58 patients who underwent limb-salvage surgery for proximal humerus tumors:
-
19 patients reconstructed with modular endoprosthesis (humeral hemiarthroplasty)
-
39 patients reconstructed with nail cement spacer
🔎 Key Findings
• Mean MSTS score:
– Endoprosthesis: 24.8 ± 1.1
– Cement spacer: 23.9 ± 1.4
→ Statistically significant difference (P = 0.018), but clinically modest
• Complication rates were comparable:
– Endoprosthesis: 26.3%
– Cement spacer: 28.2%
• No significant functional differences were observed in patients with or without axillary nerve or deltoid resection.
💡 Clinical Takeaway
Both modular endoprostheses and cement spacers provided durable limb-salvage reconstruction with nearly equivalent functional outcomes.
Importantly, our findings suggest no substantial added functional advantage of the more expensive modular endoprosthesis, particularly in settings where cost considerations are relevant.
This study supports thoughtful, individualized reconstructive decision-making based on:
-
Soft tissue status
-
Patient age and prognosis
-
Resource availability
-
Surgeon experience
📄 Outcomes of modular endoprosthesis reconstruction versus cement spacer reconstruction following resection of proximal humeral tumors
BMC Musculoskeletal Disorders (2022)
DOI: 10.1186/s12891-022-05432-4
Walid Atef Ebeid MD, Sherif Eldaw MD, Ismail Tawfeek Badr MD, Mohamed Kamal Mesregah MD, Bahaa Zakarya Hasan MD
Article links:
https://pubmed.ncbi.nlm.nih.gov/35597987/
https://link.springer.com/article/10.1186/s12891-022-05432-4
I would be interested to hear how others approach reconstruction after proximal humeral tumor resection:
-
Do you routinely favor endoprosthesis?
-
In which scenarios do you prefer cement spacers?
-
How heavily does cost influence your decision-making?
Follow the Topic
-
BMC Musculoskeletal Disorders

BMC Musculoskeletal Disorders is an open access, peer-reviewed journal that considers articles on all aspects of the prevention, diagnosis and management of musculoskeletal disorders, as well as related molecular genetics, pathophysiology, and epidemiology.
Related Collections
With Collections, you can get published faster and increase your visibility.
Environmental impacts on musculoskeletal health
BMC Musculoskeletal Disorders is calling for submissions to the Environmental impacts on musculoskeletal health collection. The Collection covers a broad range of topics related to the environmental impacts on musculoskeletal health, addressing both workplace and broader environmental factors that influence bone health and musculoskeletal diseases. Key areas of focus will include the relationship between environmental exposures and bone mineral density (BMD), as well as how poor working conditions—such as prolonged sitting, repetitive motions, and inadequate ergonomic setups—can contribute to musculoskeletal pain and disorders. The collection will also explore how occupational stress, physical strain, and environmental toxins can lead to an increased risk of fractures and musculoskeletal diseases. Additionally, it will cover emerging research on the role of ergonomic workspaces in preventing or mitigating musculoskeletal issues, emphasizing best practices for improving work environments to promote optimal musculoskeletal health.
Topics of interest include, but are not limited to:
Occupational and ergonomic exposures contributing to musculoskeletal disorders
Urbanization, physical inactivity, and access to green space as determinants of musculoskeletal health
Environmental influences on childhood skeletal development or age-related degeneration
Interactions between nutrition, environmental toxins, and bone metabolism
Geographic and socioeconomic disparities in environmental musculoskeletal risk
Policy, prevention, and public health strategies targeting environmental contributors to MSK disease.
All manuscripts submitted to this journal, including those submitted to collections and special issues, are assessed in line with our editorial policies and the journal’s peer-review process. Reviewers and editors are required to declare competing interests and can be excluded from the peer review process if a competing interest exists.
Publishing Model: Open Access
Deadline: Aug 17, 2026
Motion analysis in orthopedics
BMC Musculoskeletal Disorders is calling for submissions to the Motion analysis in orthopedics collection. The scope of this collection will cover the role of motion analysis in orthopedics, with a focus on key technologies like kinematics, pressure-mapping, and gait analysis. Articles will delve into how these tools are being used to assess joint function, movement patterns, and pressure distribution across the body, especially in the context of orthopedic surgery and rehabilitation.
Topics of interest include, but are not limited to:
The use of motion analysis in preoperative assessments.
Surgical planning.
Intraoperative monitoring to improve the precision and outcomes of orthopedic interventions.
Post-operative rehabilitation enhanced by motion analysis
Gait analysis as a tool for understanding the functional challenges of patients recovering from orthopedic surgeries, and how it informs personalized rehabilitation protocols.
Motion analysis use in evaluating the success of surgical interventions.
Pressure-mapping systems optimizing orthopedic treatments.By examining the intersection of motion analysis, technology, and orthopedic surgery, this collection will provide valuable insights into how these innovations are shaping the future of musculoskeletal medicine, improving patient outcomes, and paving the way for more effective and tailored therapeutic approaches.
All manuscripts submitted to this journal, including those submitted to collections and special issues, are assessed in line with our editorial policies and the journal’s peer-review process. Reviewers and editors are required to declare competing interests and can be excluded from the peer review process if a competing interest exists.
Publishing Model: Open Access
Deadline: Jul 20, 2026


Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in