Targeting liver cancer stem cell through EpCAM therapy targeted with chemotherapy endorse enhanced progression in hepatocellular carcinoma
Published in General & Internal Medicine
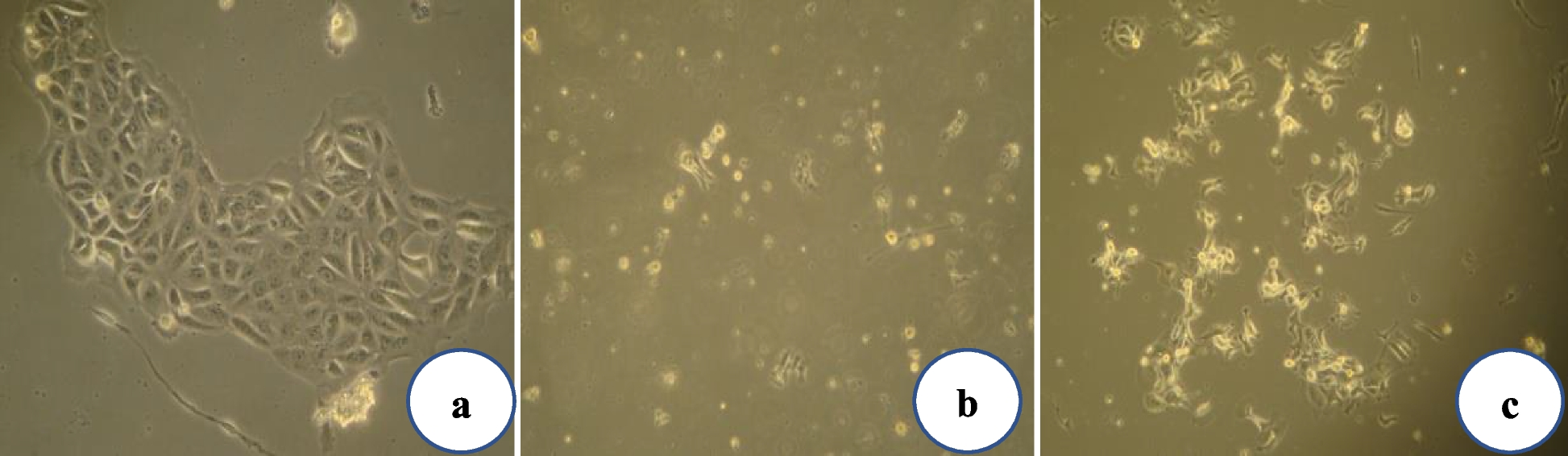
EpCAM-targeted therapy such as sh-EpCAM and XAV939 were proven to be potential inhibitors of liver cancer stem cells by inhibiting colony formation, invasion properties, and decreased expression of ABCG2, the gene responsible for chemoresistance. The LCSC expression and spheroid formation were drastically reduced in single and combination cisplatin, and EpCAM-targeted therapy. Overall, targeting EpCAM with therapies such as sh-EpCAM and XAV939 shows promise as a potential treatment for liver cancer, although further exploration is needed to regulate their efficacy and safety in clinical trials. These studies imply that combining cisplatin and EpCAM-targeted therapy may benefit both and improve cancer treatment outcomes. More research is required to determine the ideal dose, schedule, and patient selection for this combination therapy approach. It would be necessary to conduct further research to determine whether combining XAV939, EpCAM knockdown, and cisplatin could synergistically affect stem cell populations. A well-designed controlled study with appropriate sample size, randomisation, and statistical analysis is typically required to determine whether the combination of cisplatin and a specific drug has a synergistic, additive, or antagonistic effect. Research should be conducted to validate any claims regarding drug interactions to ensure that the results are accurate and reliable. These assays may provide functional evidence of the effects of the treatments on stem cell properties.