Digitising Sleep Health: A Call for Transparency and Validation
Published in Healthcare & Nursing

Sleep is essential for health and wellbeing. Although the functions of sleep are far from fully understood, it is known to promote healing, restore energy and impact both brain function and behaviour. As a result of its importance to vital human processes and the incomplete understanding of its function, accurate sleep monitoring is of interest to the understanding of human health and an active area of research.
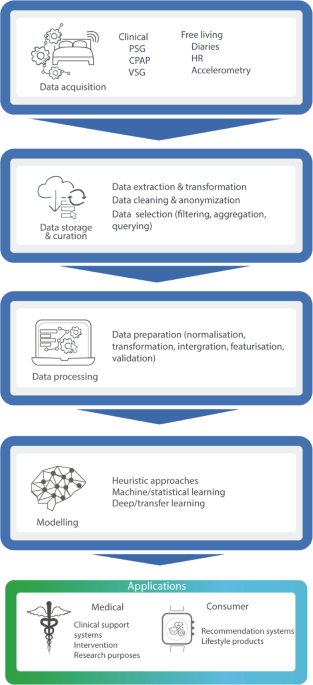
Traditionally, sleep is monitored and evaluated in laboratory settings using a technique called polysomnography (PSG). Although PSG is the gold standard for monitoring of sleep, it is burdensome, expensive and not scalable. For these reasons, a number of alternatives have emerged during recent years. In this work, we provide a multidisciplinary overview of the digitalisation of sleep, alongside the emerging technologies and modelling techniques that surround this process. To do so, we introduce the digital sleep framework, encompassing the path that sleep data takes from its acquisition to its eventual deployment in medical or consumer sleep applications. We explore the strengths and limitations of these methods, with a particular focus on data-driven approaches, such as Artificial Intelligence.

The digital sleep framework covers the path of sleep data from its acquisition to when its insights are used for medical or consumer applications.
The digitisation of sleep will have important repercussions across industry, healthcare, academia and personal health. It will facilitate more accurate sleep monitoring and may be used in early diagnosis, disease prevention or in providing lifestyle recommendations. Through this work we provide an overview of these key areas of impact and highlight the need for transparency and validation of these sleep technologies, particularly those which are commercially available. While we advocate for the opportunities introduced by these devices, we also believe that the field should proceed with caution. For example, current wrist-based wearable devices often struggle to discern between the different substages of non-REM sleep (N1,N2,N3) and REM, yet users’ may be led to interpret those inferences as factually true. These inaccuracies combined with poor sleep hygiene may exacerbate symptoms of sleep disorders such as insomnia. For some users, receiving inadequate sleep recommendations may even lead to bedtime anxiety. This calls for both proper regulation and validation of digital biomarkers related to sleep and higher levels of transparency in algorithmic development and data practices amongst industry and academic researchers working on the developments of these technologies. Together, these changes will lead to improved trust and progress, contributing to the development of validated systems for sleep health.
Follow the Topic
-
npj Digital Medicine

An online open-access journal dedicated to publishing research in all aspects of digital medicine, including the clinical application and implementation of digital and mobile technologies, virtual healthcare, and novel applications of artificial intelligence and informatics.
Related Collections
With Collections, you can get published faster and increase your visibility.
Evaluating the Real-World Clinical Performance of AI
Publishing Model: Open Access
Deadline: Jun 03, 2026
Impact of Agentic AI on Care Delivery
Publishing Model: Open Access
Deadline: Jul 12, 2026


Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in