Blood pressure control with active ultrafiltration measures and without antihypertensives is essential for survival in hemodiafiltration and hemodialysis programs for patients with CKD. A prospective observational study.
Published in Social Sciences, General & Internal Medicine, and Pharmacy & Pharmacology
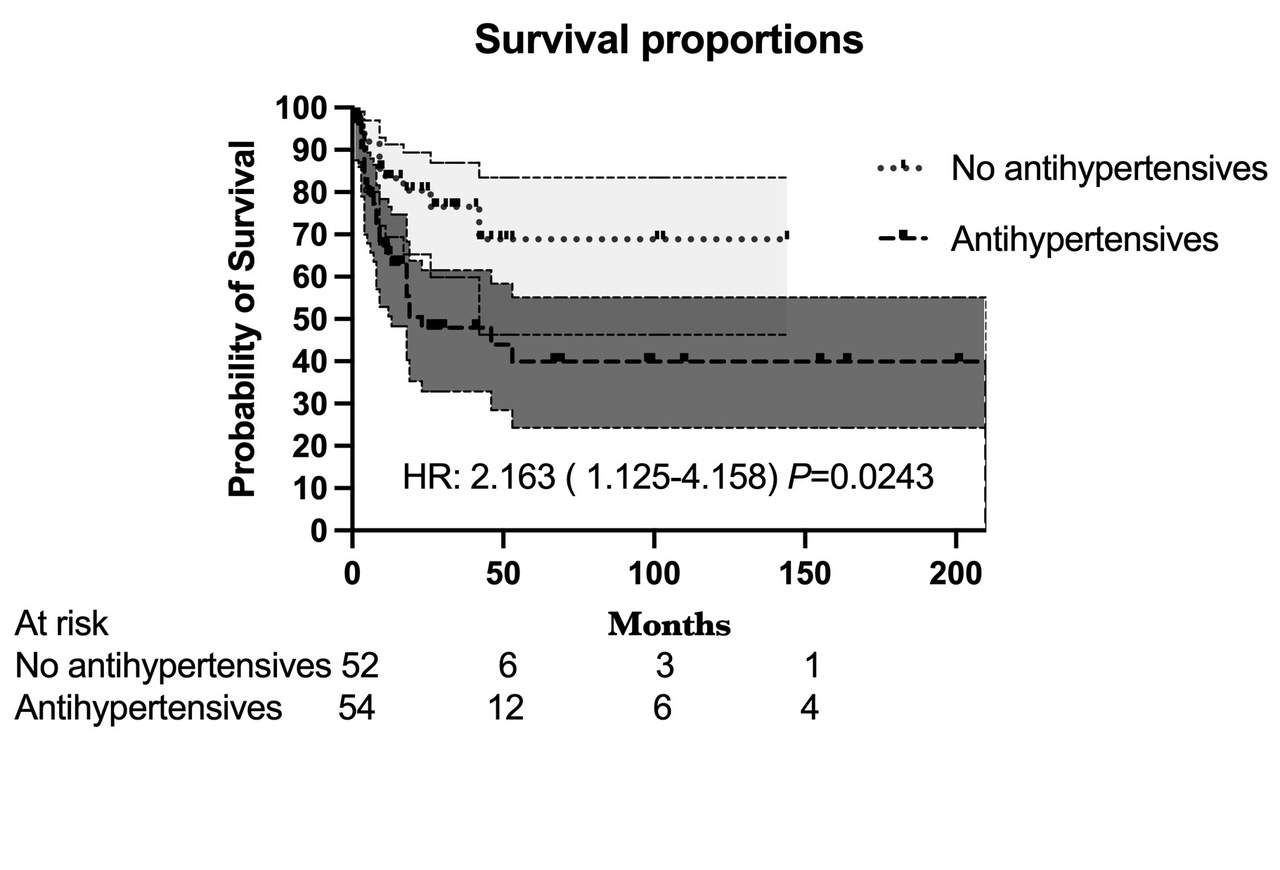
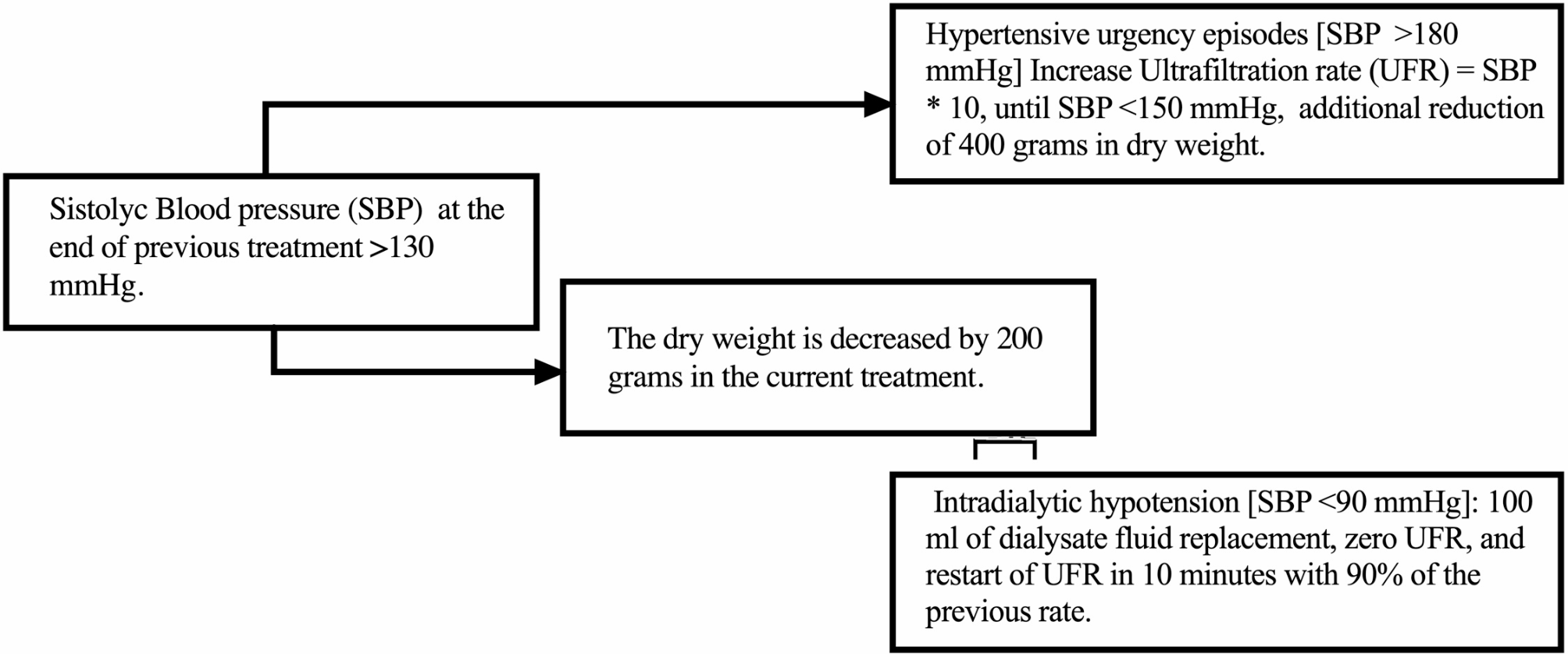
The main finding confirms the hypothesis of the study that there is more remarkable survival in the group of patients with CKD whose hypertension can be controlled without antihypertensive treatment and with the use of constant dry weight reduction measures to optimize ultrafiltration. The factors associated with the lack of control of arterial hypertension were a history of vascular amputation, a history of being an ex-smoker, being a carrier of type 2 diabetes mellitus, having a serum ferritin level greater than 26.75%, being male, and being treated with hemodialysis. The associated protective factors were having a diagnosis of glomerulonephritis as an etiology of chronic kidney disease, a history of never smoking, a serum ALB concentration greater than 4.214 g/dl, effective blood flow greater than 423.5 ml/min, and interdialytic weight gain >4.925%, hemodiafiltration as treatment, urea levels less than 103.78 mg/dl, and fasting glucose levels less than 109.2 mg/dl. According to the time-adjusted model, only four factors were associated: age, transferrin saturation, serum albumin levels, and history of vascular amputation.
In the stratified analysis, differences in survival were demonstrated by the percentiles of blood pressure taken in the last month of survival or censoring. With blood pressures ranging from 141 mmHg to 122 mmHg, there is a proportional risk of death associated with the intake of antihypertensive agents. The same occurs when the blood pressure is less than 105 mmHg. These relationships could not be established with pressures greater than 141 mmHg.
Follow the Topic
-
BMC Nephrology

This is an open access journal publishing original peer-reviewed research articles in all aspects of the prevention, diagnosis and management of kidney and associated disorders, as well as related molecular genetics, pathophysiology, and epidemiology.
Your space to connect: The Cancer in understudied populations Hub
A new Communities’ space to connect, collaborate, and explore research on Cancers, Race and Ethnicity Studies and Mortality and Longevity!
Continue reading announcementRelated Collections
With Collections, you can get published faster and increase your visibility.
Robotic surgery: clinical application in nephrology
BMC Nephrology is calling for submissions to our Collection on Robotic surgery: clinical application in nephrology.
Robotic surgery has emerged as a transformative approach in the field of nephrology, enabling surgeons to perform complex procedures with enhanced precision and control. With the advent of advanced robotic systems, such as the da Vinci Surgical System, urologists are now able to tackle intricate renal surgeries that were previously deemed challenging with traditional methods. As the technology continues to evolve, its applications in nephrology are expanding, paving the way for innovative surgical practices.
The integration of robotic surgery into nephrology is of critical importance as it addresses the increasing demand for effective and less invasive treatment options for renal diseases. Recent advancements in robotic technology have led to improved dexterity and visualization during surgery, allowing for greater surgical accuracy. The continuous development in this field not only promises enhanced surgical outcomes but also positions robotic surgery as a key player in the future of renal care.
Topics of interest include, but are not limited to:
Applications of da Vinci surgery in nephrology
Innovations in robotic microsurgery
High-tech surgery techniques in renal procedures
Future directions in robotics in medicine
This Collection supports and amplifies research related to SDG 3 (Good Health and Well-being) and SDG 9 (Industry, Innovation, and Infrastructure).
All manuscripts submitted to this journal, including those submitted to collections and special issues, are assessed in line with our editorial policies and the journal’s peer review process. Reviewers and editors are required to declare competing interests and can be excluded from the peer review process if a competing interest exists.
Publishing Model: Open Access
Deadline: May 22, 2026
Novel therapies for glomerular diseases
BMC Nephrology invites submissions to our Collection on Novel therapies for glomerular diseases.
Glomerular diseases encompass a diverse group of disorders that affect the kidney's filtering units, leading to significant morbidity and mortality. These conditions, which include focal segmental glomerulosclerosis, minimal change disease, and IgA nephropathy, have traditionally posed challenges in terms of effective treatment options. Recent advancements in our understanding of the underlying pathophysiology and the introduction of novel therapeutic modalities, such as targeted biologics and small molecules, present new avenues for intervention. This Collection invites contributions that explore these innovative therapies and their potential to transform the management of glomerular diseases.
Advances in clinical research have led to promising developments, including the successful completion of several clinical trials that evaluate the efficacy of new agents. These therapies not only aim to improve patient outcomes but also focus on personalized treatment approaches that consider individual patient characteristics. By fostering collaboration among researchers, clinicians, and industry partners, we can enhance our understanding and management of these complex conditions. Continued research in this field has the potential to yield groundbreaking discoveries that could redefine treatment paradigms for glomerular diseases.
Topics of interest for this Collection include, but are not limited to:
Novel therapeutic agents in glomerular diseases
Clinical trials of innovative treatments
Impact of new therapies on patient outcomes
Personalized treatment approaches for glomerular disorders
This Collection supports and amplifies research related to SDG 3: Good Health and Well-being and SDG 9: Industry, Innovation, and Infrastructure.
All manuscripts submitted to this journal, including those submitted to collections and special issues, are assessed in line with our editorial policies and the journal’s peer review process. Reviewers and editors are required to declare competing interests and can be excluded from the peer review process if a competing interest exists.
Publishing Model: Open Access
Deadline: Jun 30, 2026

Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in