Centenarians: Who They Are and What We've Learned
Published in Paediatrics, Reproductive Medicine & Geriatrics
Question of This Study
Centenarians, who reach the remarkable age of 100, have become more common over the years, but we don't know much about them. This study sought to uncover the characteristics of Sweden's centenarian population, shedding light on their living arrangements, socio-demographic profiles, health, and geriatric care, meaning formal home care or residing in a care home.
Study Findings
- Who Are Sweden's Centenarians?
- Mostly Women: Of the 5,882 centenarians studied, the majority (81%) were women, emphasizing the remarkable longevity of the female population.
- Living Arrangements: Many centenarians (40%) lived alone, while a small proportion (8%) cohabited. The rest of the centenarians lived in care homes (52%). Male centenarians (18%) were more likely to cohabitate than female centenarians (6%).
- Familial Proximity: About 67% had a child living within a 50 km radius.
- Income: The majority (77%) had incomes below the median for older adults in Sweden, highlighting economic vulnerability.
- Health Status of Centenarians (Figure1)
- Comorbidities: Over half of the centenarians had at least one chronic health condition, with 1 out of 3 experiencing multiple health issues. Heart failure was the most common diagnosis, followed by myocardial infarction and cerebrovascular disease.
- Prescribed Medications: Almost none were free from drugs, with a high proportion of polypharmacy (Men, 62%; Women, 66%), indicating a substantial medication load.
- Gender Difference: Women received more prescribed drugs than men, although men had more morbidities.
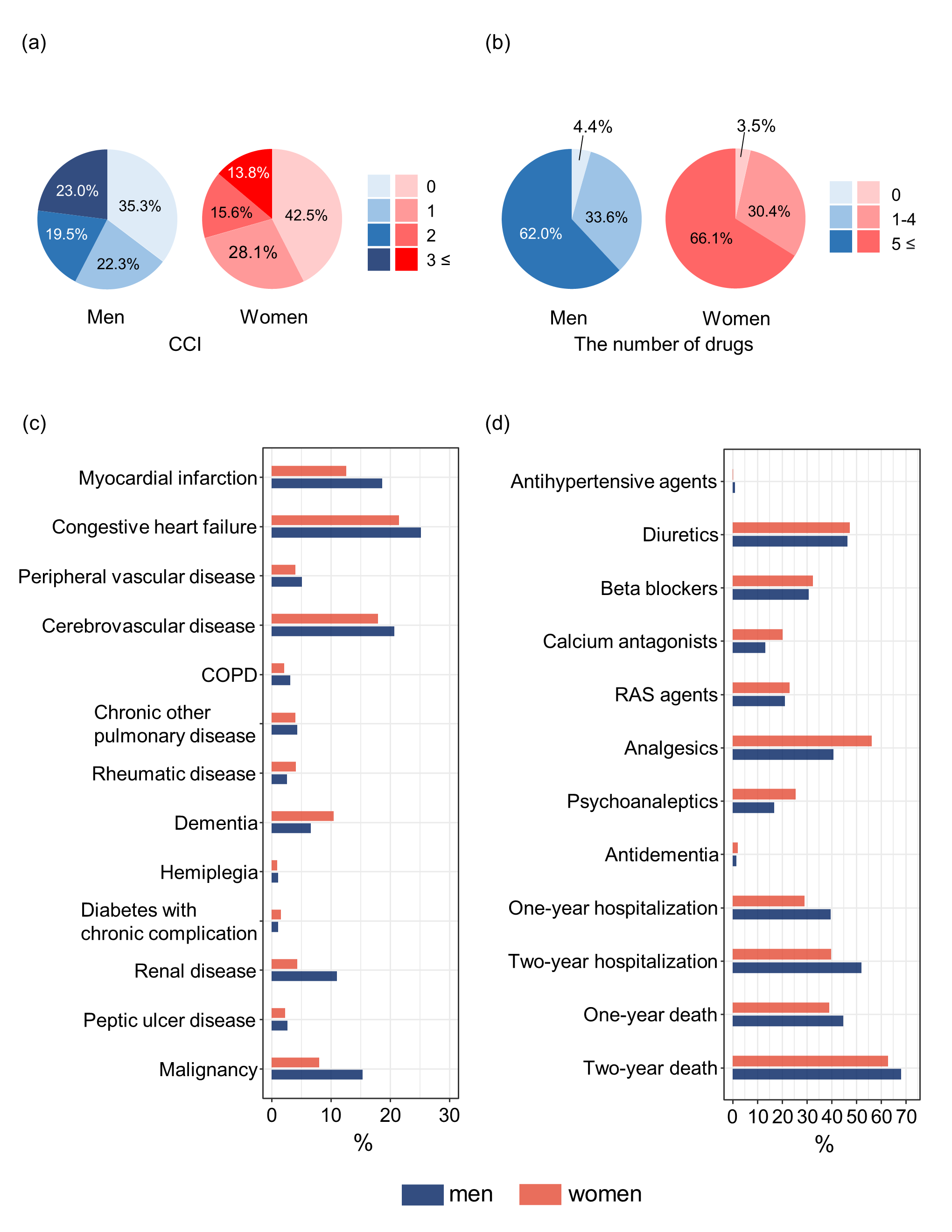
CCI Charlson comorbidity index, COPD Chronic obstructive pulmonary disease, RAS Renin-angiotensin system
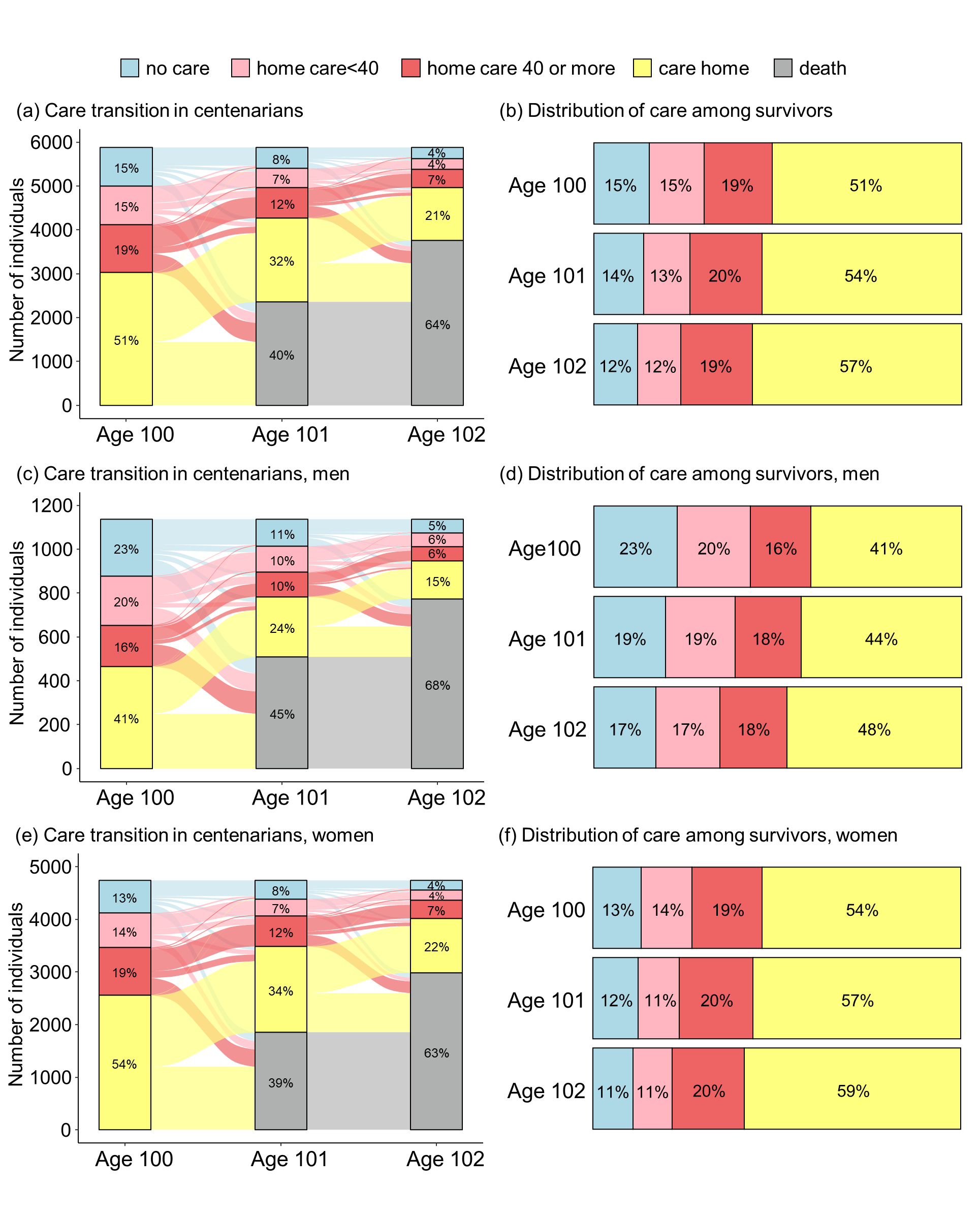
- Geriatric Care Transitions (Figure2)
- Care Homes: Roughly half of centenarians at the age of 100 resided in care homes, with a higher proportion of women (54%) than men (41%).
- Care Needs: Two years later, only 4% continued to live at home without formal care, while 64% had passed away.
Conclusion
Sweden's centenarian population is not characterized by exceptional health or independence. Instead, they face many health issues, polypharmacy, and a heavy reliance on geriatric care. With most centenarians living alone and having limited incomes, they belong to a vulnerable demographic group. Strategies need to be devised and implemented to address the healthcare and social support demands of this growing population. Only 2% of the centenarians had no diagnosed morbidity, a maximum of 1 drug, and no geriatric care. This study provides valuable insights into the lives of centenarians, dispelling the myth that they are uniformly healthy and independent. As the number of centenarians continues to rise, understanding their unique needs and challenges becomes increasingly critical for healthcare and social services planning.
Follow the Topic
-
Aging Clinical and Experimental Research

This journal offers a multidisciplinary forum on the progressing field of gerontology and geriatrics. The areas covered by the journal include: biogerontology, neurosciences, epidemiology, clinical gerontology and geriatric assessment, social, economical and behavioral gerontology.
Related Collections
With Collections, you can get published faster and increase your visibility.
Low Back Pain in Older Adults: A Multidisciplinary Approach to Care and Prevention, with ESCEO Collaboration
Aging Clinical and Experimental Research (ACER) is dedicated to advancing knowledge on aging-related health challenges. Low back pain (LBP) is a leading cause of disability and reduced quality of life in adults, with its impact increasing with age due to degenerative changes and comorbidities. Manuscripts exploring the following themes are particularly encouraged:
1. Epidemiology and Burden of Low Back Pain
Prevalence, risk factors, and socioeconomic burden of LBP in adult populations.
Impact of chronic LBP on mobility, function, and quality of life.
Occupational and lifestyle contributions to LBP development.
2. Pathophysiology and Age-Related Changes
Degenerative processes affecting spinal health, including intervertebral disc degeneration, facet joint arthritis, spinal stenosis and sarcopenia
Neuromuscular and vascular changes influencing pain perception and chronicity
The role of osteoporosis and vertebral fractures in LBP progression
3. Comprehensive Assessment and Diagnosis
Clinical evaluation and red flag symptoms in adults with LBP
Advancements in imaging and diagnostic modalities for differentiating LBP etiologies
Challenges in diagnosing LBP in middle-aged and older adults with multiple comorbidities
4. Multimodal Management and Treatment Strategies
Pharmacological interventions: Balancing efficacy, safety, and polypharmacy concerns
Non-pharmacological approaches: Physical therapy, exercise-based interventions (e.g., yoga, tai chi), hydrotherapy, and manual therapy
Minimally invasive treatments: Epidural steroid injections, radiofrequency ablation, and regenerative medicine therapies
Surgical considerations: Indications, outcomes, and risks for adults undergoing spinal surgery
5. Prevention, Rehabilitation, and Long-Term Care
Strategies for reducing disability and promoting functional independence
Ergonomic modifications and workplace interventions for preventing LBP
Role of digital health solutions, telemedicine, and wearable technology in long-term LBP management
Health disparities and access to LBP treatment among diverse adult populations
Call for Research Contributions
ACER invites original research articles, reviews, and clinical studies that enhance the understanding, management, and prevention of low back pain in adults. By addressing this critical issue, the journal aims to foster multidisciplinary approaches that improve patient outcomes and quality of life across the aging continuum.
KEYWORDS: Low back pain, Musculoskeletal health, Spinal degeneration, Pain management, Older spine, Physical therapy
Publishing Model: Open Access
Deadline: Ongoing



Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in