Longitudinal observation and decline of neutralizing antibody responses in the three months following SARS-CoV-2 infection in humans
Published in Microbiology

In mid-March 2020 SARS-Cov-2 had forced the UK into lockdown and most labs in our department were preparing to pause their research and close. Instead of going home to write unfinished papers, the Doores lab were collecting reagents from old and new collaborators. Our ongoing research on studying the antibody response to HIV-1, hantaviruses and phleboviruses had equipped us to switch our focus quickly to SARS-Cov-2. The efforts in the subsequent months culminated in our recently published article in Nature Microbiology detailing the evaluation of longitudinal serum samples from people infected with SARS-Cov-2.
We first set out to establish serology assays and neutralisation assays to assist our clinical colleagues at St Thomas’ with diagnostics. At the time it was a surreal experience, travelling through the empty streets of central London to work in an almost vacant lab (Figure 1). The usually busy department had been reduced to a skeleton crew with many students and post-docs being relocated to St Thomas’ Hospital to assist in sample handling and curation. We soon discovered that sequential serum samples were being collected as part of the routine clinical care hospitalized COVID-19 patients were receiving and we therefore set out to study the kinetics, magnitude and longevity of antibody responses following SARS-CoV-2 infection. Our colleagues also had the foresight to seek ethical approval to collect sequential serum samples from healthcare workers at the hospital thus providing the perfect opportunity to compare antibody responses across a very wide range of COVID-19 related disease severities.

A routine ELISA for us would usually involve a couple of plates once every few weeks. However, for this study we were required to set up 10-20 plates every day. With so many plates accumulated over the course of this work we were able to build an impressive multi layered wall of ELISA plates in our lab (Figure 2). cater for this increased workload our lab team had to expand, and we recruited new members from the large community of students and post-docs tired of working on their computers. With the extra help we were able carry out neutralisation assays with both pseudotyped virus and authentic virus on our serum samples.
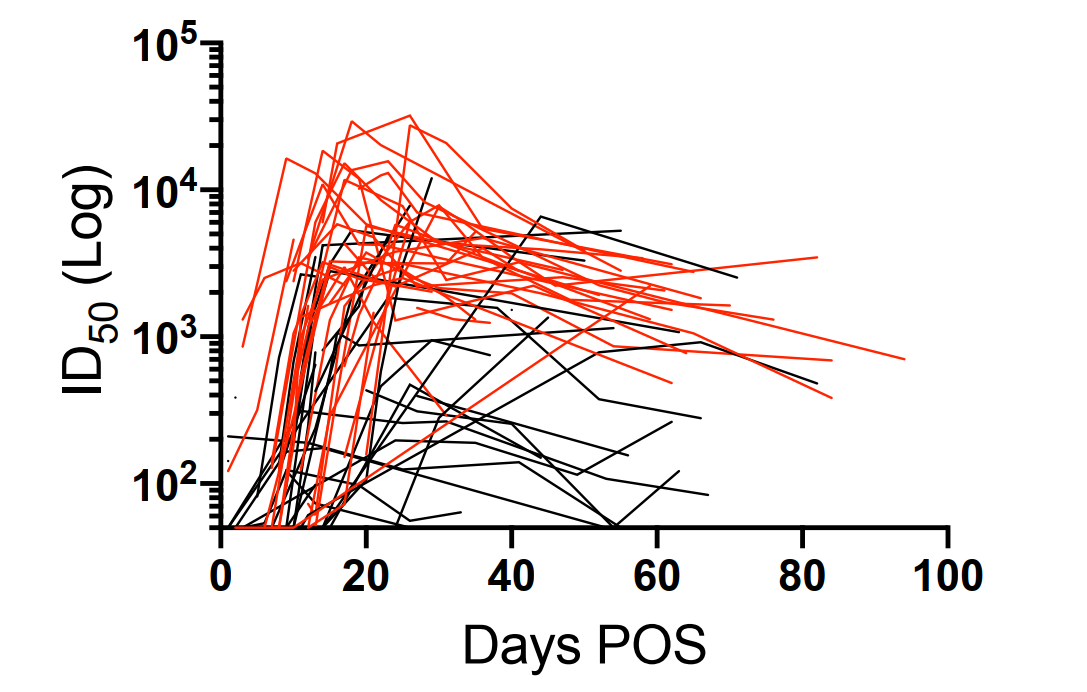
These results showed that in our cohort the neutralising antibody response declined over the first 3 months following infection. (Figure 3) Additionally, severity of the disease seemed to affect the magnitude of the neutralising response. Hence, asymptomatic carriers who had a lower peak level of antibodies approached the limits of the assay detection in later timepoints. The kinetics of the antibody response we observed were typical of acute viral infection and comparable to the response elicited from seasonal coronaviruses. Our observations suggest that SARS-CoV-2 vaccines should aim to elicit an immune response similar to that elicited by severe disease and may require boosting to maintain neutralising antibody titres. Although our work gives a clearer insight into the immune response to SARS-Cov-2 over time, it is still unknown whether titres will continue to wane beyond 3 months or plateau at a stable level for a sustained period. Furthermore, it is still unclear what titre of neutralising antibodies is required for protection from infection or disease, hence, further research is required.
Follow the Topic
-
Nature Microbiology

An online-only monthly journal interested in all aspects of microorganisms, be it their evolution, physiology and cell biology; their interactions with each other, with a host or with an environment; or their societal significance.
Related Collections
With Collections, you can get published faster and increase your visibility.
The Clinical Microbiome
Publishing Model: Hybrid
Deadline: Mar 11, 2026



Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in