No Evidence of Disease in patients with HER2-positive metastatic breast cancer – can some patients stop treatment?
Published in Cancer

HER2-positive breast cancer comprises ~15-20% of new breast cancer diagnoses with 25% of patients presenting with de novo (newly diagnosed) metastatic disease and 3-30% relapsing within 5 years depending on stage1,2. The humanized monoclonal antibody trastuzumab was the first biomarker-driven targeted therapy in solid tumours, improving the survival of patients with both early and metastatic HER2-positive breast cancer. In the 20 years since trastuzumab’s discovery, a plethora of increasingly efficacious HER2-targeted therapies (eg: pertuzumab, trastuzumab-emtansine, trastuzumab-deruxtecan, tucatinib) continue to improve survival for patients with HER2-positive metastatic breast cancer3, which now exceeds four years. As HER2-targeting improves, an increasing yet small proportion of patients (~1-6%) will experience superior and often durable tumor response, exemplified by complete radiographic (eg: CT scan, bone scan) resolution of their visual cancer burden. In the context of a clinical trial, this tumor resolution is termed a complete response (CR), or outside of a clinical trial is similarly described as “no evidence of disease” (NED). Although the factors that influence CR/NED and long-term disease control are not fully understood, improvements in HER2-targeting and immune engagement are thought to play pivotal roles and are active areas of investigation4.
It is currently unknown whether visual resolution of HER-positive metastatic tumor burden on CT is also indicative of eradication of microscopic disease. Due to this clinical equipoise, patients often continue indefinitely on HER2-targeted therapy, sometimes for decades despite having no measurable disease. This not only lends the opportunity for drug toxicity (eg: heart failure, intractable diarrhea) with individual treatments, but also compounds financial toxicities as HER2 antibodies are often combined with other costly HER2-targeted agents and administered indefinitely every three weeks. Thus, evaluating the clinical and pathologic factors of patients on HER2-targeted therapy that influence long-term response and identifying those that could potentially discontinue HER2 treatment in lieu of ongoing surveillance, would be of substantial benefit.
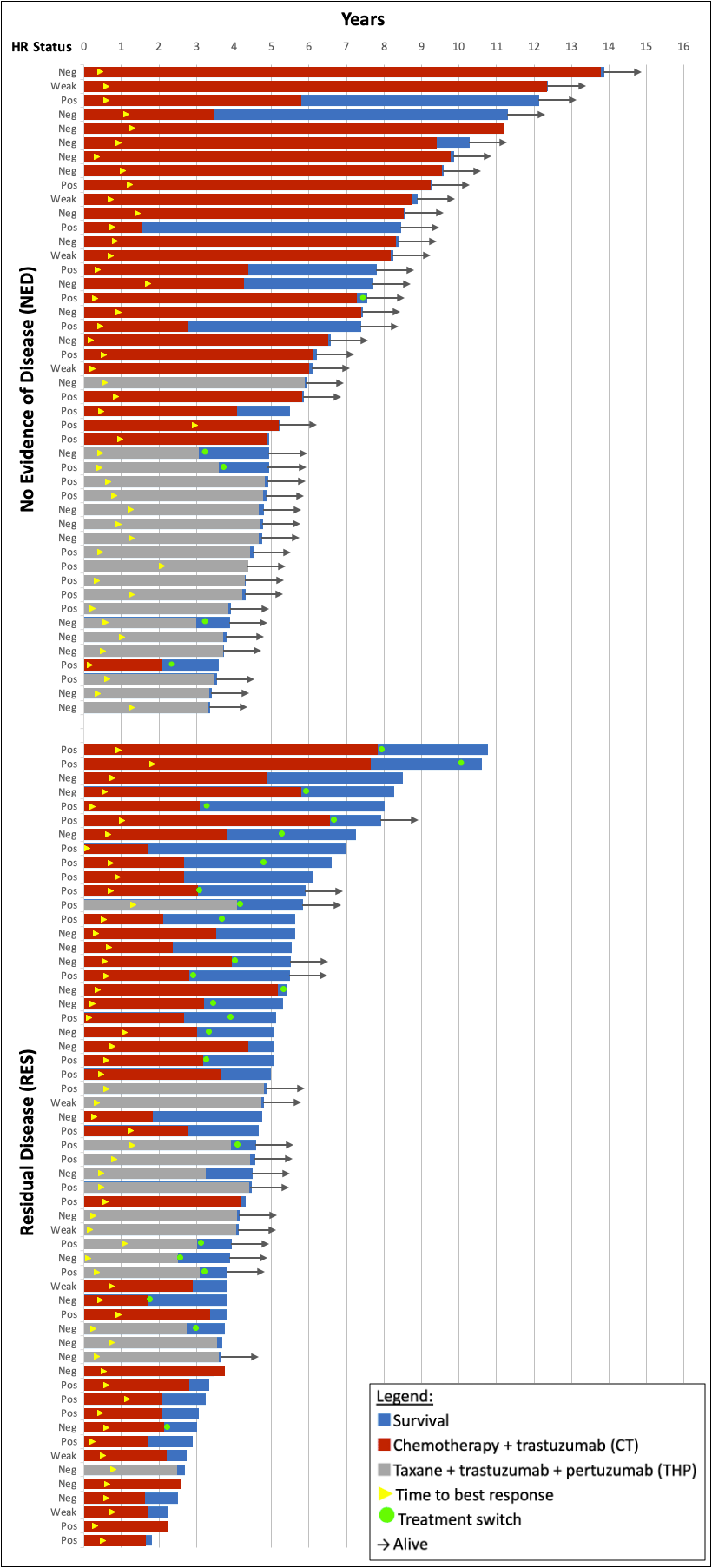
The main objective of our multi-institution, retrospective study5 was to compare the clinical characteristics of patients receiving first-line HER2 targeted therapy from 2005 to 2016 with long-term response. Patients were grouped into those experiencing no evidence of disease (NED) versus those with residual disease (RES) on sequential CT and/or bone scans. Patients with HER2- positive metastatic breast cancer receiving either (1) chemotherapy-trastuzumab (CT) or (2) taxane-trastuzumab-pertuzumab (THP) at Princess Margaret Cancer Center in Toronto, Ontario, or in the province of Alberta were included. The clinical characteristics of eligible patients were then evaluated for association with progression and/or survival in addition to their association with NED.
Of 103 patients with metastatic HER2- positive breast cancer meeting eligibility criteria, 46 achieved NED and 57 had RES. For patients with NED, 97.4% survived 5-years and 85.7% survived 10-years. Comparatively for RES, 61.3% survived 5-years and 9.4% survived to the 10-year cut-off. Of all clinical variables, only NED was significantly associated with improved survival, whereas pre-menopausal status, de novo metastatic disease, and no palliative radiotherapy were associated with achieving NED. Perhaps most striking were 6 of 7 patients (85.7%) with NED who discontinued HER2 therapy for >1 year and were alive and without evidence of recurrence, relative to 1 of 17 (5.9%) in the RES group.
As HER2 targeting improves, so does the proportion of patients achieving CR/NED and long-term survival. In the recently reported DESTINY-Breast03 study6 using the drug-antibody conjugate trastuzumab-deruxtecan, 8.7% of patients demonstrated a complete response to therapy. Moreover, in final analyses of the CLEOPATRA trial using chemotherapy in combination with trastuzumab and pertuzumab, 16% of patients were without progression (remaining on treatment) and 37% of patients were alive at 8 years7. With increasing individual drug costs compounded by multi-agent HER2 regimens, longer survival, and indefinite treatment, the identification of clinical (eg: NED) and/or molecular biomarkers (eg: ctDNA) to facilitate safe treatment discontinuation in lieu of surveillance has become paramount within publicly funded healthcare systems. Moreover, the cost savings achieved from identifying and applying such biomarkers, may allow for the re-allocation of cancer-care funds and access to new or underfunded therapies.
In summary, patients achieving NED have superior survival relative to patients with residual disease on diagnostic imaging. Pre-menopausal patients with de novo metastatic disease are more likely to achieve NED and may be optimal candidates for surveillance strategies. Further studies are needed to identify reliable molecular biomarkers and safe surveillance strategies for this small, yet increasing group of patients.
References:
- Howlader N, Cronin KA, Kurian AW, Andridge R. Differences in breast cancer survival by molecular subtypes in the United States. Cancer Epidemiology Biomarkers and Prevention. 2018;27(6). doi:10.1158/1055-9965.EPI-17-0627
- Chumsri S, Li Z, Serie DJ, Mashadi-Hossein A, Colon-Otero G, Song N, Pogue-Geile KL, Gavin PG, Paik S, Moreno-Aspitia A, Perez EA, Aubrey Thompson E. Incidence of late relapses in patients with HER2-positive breast cancer receiving adjuvant trastuzumab: Combined analysis of NCCTG N9831 (Alliance) and NRG oncology/NSABP B-31. Journal of Clinical Oncology. 2019;37(35). doi:10.1200/JCO.19.00443
- Martínez-Sáez O, Prat A. Current and Future Management of HER2-Positive Metastatic Breast Cancer. JCO Oncology Practice. 2021;17(10). doi:10.1200/op.21.00172
- Griguolo G, Pascual T, Dieci MV, Guarneri V, Prat A. Interaction of host immunity with HER2-targeted treatment and tumor heterogeneity in HER2-positive breast cancer. Journal for ImmunoTherapy of Cancer. 2019;7(1):90. doi:10.1186/s40425-019-0548-6
- Veitch Z, Ribnikar D, Tilley D, Tang PA, King K, Bedard PL, Lupichuk S, Cescon DW. No evidence of disease versus residual disease in long-term responders to first-line HER2-targeted therapy for metastatic breast cancer. British Journal of Cancer. Published online December 20, 2021. doi:10.1038/s41416-021-01676-4
- Cortés J, Kim SB, Chung WP, Im SA, Park YH, Hegg R, Kim MH, Tseng LM, Petry V, Chung CF, Iwata H, Hamilton E, Curigliano G, Xu B, Lee C, Liu Y, Cathcart J, Bako E, Verma S, Hurvitz SA. LBA1 Trastuzumab deruxtecan (T-DXd) vs trastuzumab emtansine (T-DM1) in patients (Pts) with HER2+ metastatic breast cancer (mBC): Results of the randomized phase III DESTINY-Breast03 study. Annals of Oncology. 2021;32. doi:10.1016/j.annonc.2021.08.2087
- Swain SM, Miles D, Kim SB, Im YH, Im SA, Semiglazov V, Ciruelos E, Schneeweiss A, Monturus E, Clark E, Knott A, Restuccia E, Benyunes M, Cortes J. End-of-study analysis from the phase III, randomized, double-blind, placebo (Pla)-controlled CLEOPATRA study of first-line (1L) pertuzumab (P), trastuzumab (H), and docetaxel (D) in patients (pts) with HER2-positive metastatic breast cancer (MBC). Journal of Clinical Oncology. 2019;37(15_suppl):1020-1020. doi:10.1200/JCO.2019.37.15_suppl.1020
Follow the Topic
-
British Journal of Cancer

This journal is devoted to publishing cutting edge discovery, translational and clinical cancer research across the broad spectrum of oncology.



Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in