Religiosity Weakens Gaming Disorder Risk
Published in General & Internal Medicine and Behavioural Sciences & Psychology

Study overview
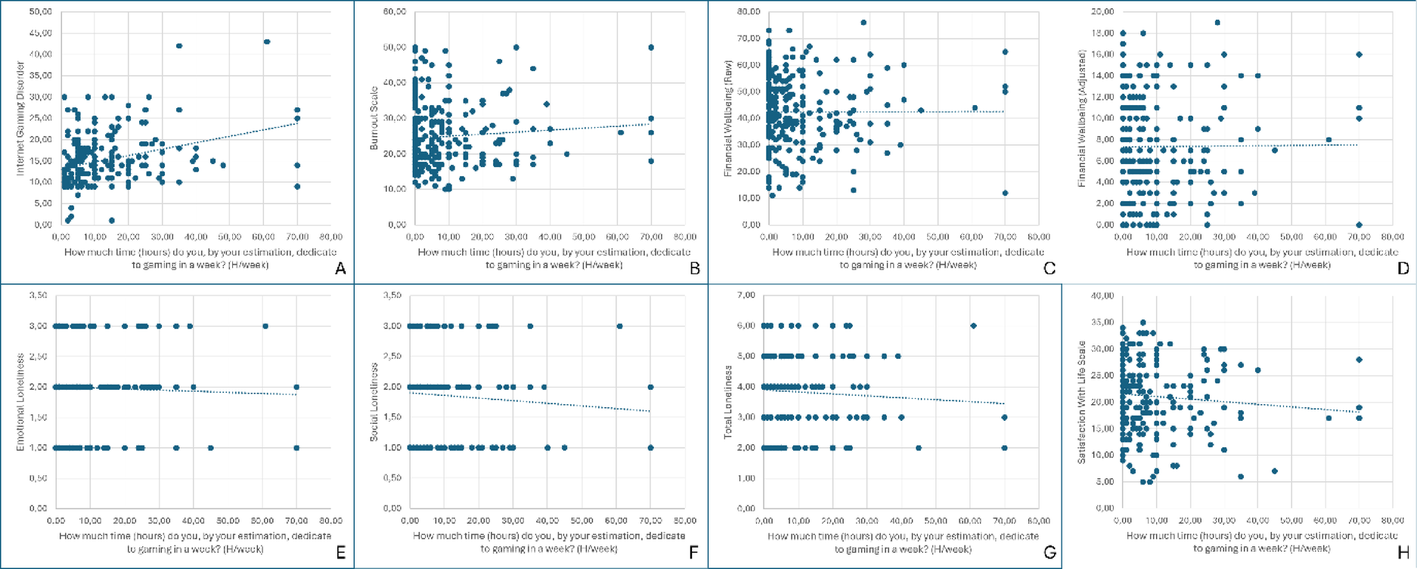
This work explores how weekly gaming duration relate to mental health outcomes in young university students in Georgia. We assessed gaming hours alongside IGD severity, burnout, loneliness, life satisfaction, financial wellbeing, and self-reported religiosity.
Although overall gaming time in our sample was modest (mean ≈ 8 hours/week), increased gaming hours were associated with higher IGD severity. Male students demonstrated significantly higher IGD scores than female students.
A protective role of religiosity
One of the central findings is that religiosity may act as a protective factor. Students with higher religiosity reported lower IGD severity, and religiosity moderated the relationship between gaming hours and IGD symptoms. This suggests that cultural and psychosocial resources could buffer some of the risks associated with problematic gaming behaviour.
Collaboration
The study was conducted in partnership with the RADAR Center at Ben-Gurion University of the Negev (Israel). Working with RADAR allowed us to integrate a broader cross-cultural perspective on digital behavior and mental health, and strengthened the methodological and analytical framework of the project. This collaboration highlights the importance of multidisciplinary and international teamwork in understanding emerging behavioral health challenges.
Why this matters
Most evidence on IGD originates from Western Europe, North America, and East Asia. Our data add insights from the Caucasus region, where cultural norms—including the role of faith communities—may shape coping strategies, socialization, and digital behavior. These findings offer valuable context for public health planning and student mental-health services.
Future directions
We anticipate that longitudinal and interventional research will clarify causal pathways (e.g., whether gaming intensity predicts burnout or vice-versa), and test whether community- or faith-based engagement can mitigate IGD-related harms in young adults.
We welcome discussion, replication efforts, and collaborative work—particularly comparisons across countries and cultures interested in youth mental health, digital behavior, and protective psychosocial factors.
Follow the Topic
-
Discover Mental Health

This is an international, open access journal that publishes research across the transdisciplinary field of mental health research.
Related Collections
With Collections, you can get published faster and increase your visibility.
Advancing Mental Health through Nursing Innovations in Care, Research, and Education
This Collection invites cutting-edge research and perspectives on advancing mental health systems by empowering nurses through innovations in clinical care, research, and education. Nurses play a pivotal role in mental health delivery, yet their own well-being and professional development are critical to sustaining high-quality patient outcomes. This Collection seeks interdisciplinary contributions that explore novel strategies to enhance nurses’ mental health resilience, optimize evidence-based practices, and foster transformative educational frameworks. Topics of interest include (but are not limited to):
• Innovative care models (e.g., trauma-informed care, digital health tools, workplace interventions).
• Research advancements in psychiatric nursing, including interdisciplinary collaborations and policy-driven studies.
• Educational initiatives addressing burnout prevention, skill development, and lifelong learning.
• Strategies to promote nurses’ psychological well-being and organizational support systems.
We welcome original research, reviews, and case studies that bridge theory and practice, with a focus on scalability and global applicability. Submissions emphasizing equity, interprofessional collaboration, and measurable impacts on both nurse and patient outcomes are particularly encouraged.
Keywords:
Nurse mental health, psychiatric nursing innovations, care models, workplace well-being, nursing education, interprofessional collaboration, digital health, resilience, evidence-based practice.
Publishing Model: Open Access
Deadline: Mar 31, 2026
Neurocognitive Disorders Beyond Cognition: Behavioral, Psychological, and Social Dimensions
Neurocognitive disorders, including mild cognitive impairment (MCI) and dementia, are defined by cognitive decline. However, their clinical reality extends far beyond cognitive symptoms. Behavioral and psychological manifestations are highly prevalent, and often more distressing for patients and caregivers than cognitive decline itself. These symptoms accelerate functional deterioration, increase caregiver burden, and contribute to poor quality of life and higher healthcare costs.
This Special Collection seeks to highlight the behavioral, psychological, and social dimensions of neurocognitive disorders, bridging biological mechanisms, clinical management, psychosocial outcomes, and health policy. In particular, it aims to explore how the digital health and policy innovations can make a meaningful impact.
We invite research that explores how digital health, AI, and telemedicine can advance assessment, intervention, and care models, as well as studies that inform policy and service delivery. Submissions may include original research, systematic reviews, methodological papers, and policy analyses from psychiatry, neurology, psychology, geriatrics, and related fields.
Scope
1. Behavioral and Psychological Symptoms – Neuropsychiatric manifestations (e.g., depression, apathy, agitation, aggression, delusions, hallucinations) in dementia and MCI, their mechanisms, clinical correlates, and psychosocial Impact (e.g., on quality of life, caregiver burden, stigma, social participation).
2. Interventions – Pharmacological, psychosocial, lifestyle-based, and digital interventions (e.g., app-based therapies, AI-assisted care) targeting behavioral, psychological, and social needs.
3. Policy and Care Models – Service innovations and policy frameworks, including the integration of digital platforms, AI-supported systems, and telemedicine in dementia and MCI care.
Keywords: dementia, major neurocognitive disorder, mild neurocognitive disorder, mild cognitive impairment, behavioral and psychological symptoms of dementia, Neuropsychiatric manifestations
Publishing Model: Open Access
Deadline: Jun 15, 2026

Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in
This is very interesting and relevant paper in this decades. Gaming disorder significantly increases in the few recent years. Findings of this article may provide valuable information to prevent the risk of gaming disorder.
Thank you, the international cooperation is moving forward with gathering multicultural data and analysis. More papers to come.