Behind the Paper: “Molecular Disparities in Colorectal Cancers of White Americans, Alabama African Americans, and Oklahoma American Indians”
Published in Cancer
Link to the paper:
https://www.nature.com/articles/s41698-023-00433-5
Race is a sensitive subject in biomedical science and an important covariate in cancer outcomes
Humans are often categorized into races. Historically, racism (i.e., discrimination and prejudice towards people based on their race or ethnicity) has existed, as has anti-racism viewpoints. In the biomedical field, the social context has made the issue of race a sensitive subject. The conflict among viewpoints can be a barrier to the evaluation of biological race in an unbiased manner.
We posit that ethnic/racial groups share biological patterning that occurs because of social constructs, as well as dietary habitats, geographic locations, and other cultural practice and lifestyles. With recent technological advancements, biomedical research tools are available to identify, at the molecular level, such biological patterning among races.
Colorectal cancer (CRC) and outcomes from the standpoint of race
In the USA, colorectal cancer (CRC) is the third most common cancer diagnosed in men and women. The 5-year survival rate for localized CRC is 91%, but the rate drops to 72% (regional) and 13% (distant/metastatic); thus, CRC is a major threat to public health.
Cancer epidemiology and disparity studies show that the outcomes of CRC differ among racial groups. Blacks/African Americans (AAs) have poorer outcomes, as do American Indians (AIs) in Oklahoma (USA), where this new study was conducted.
Our plan: investigate molecular disparities in CRCs among whites, Blacks/AAs, and AIs
We hypothesized that differences between racial groups explain, in part, these disparities in CRC outcomes. To test this hypothesis, we analyzed CRCs and normal/benign colon tissue at the molecular level (i.e., transcriptome, mutational profiling of CRCs and/or germline [normal-looking/benign] genomic DNA).
Sample procurement difficulties
With a team of bioinformatics analysts, a molecular biologist, a cancer biologist, and a sequencing/genomics core facility, molecular profiling of cancer and comparisons among groups was technologically feasible at our institute. For Alabama AAs, Dr. Manne has established a bio-depository at the University of Alabama, Birmingham (UAB), and his group provided samples for whites and AAs.
We were aware, however, that collecting other samples could be difficult. Concerning CRC samples from Oklahoma AIs, many AI tribes see the human body as sacred, and requests for biospecimens can be met with reluctance. Historical and ongoing racial discrimination contribute to a concern for data mis-representation. Hospitals in tribal territories may not have specimen collection programs for research purposes. Nonetheless, in collaboration with Dr. Morris, Department of Surgery, University of Oklahoma Health Sciences Center, we initiated the present analysis with hope that it would provide preliminary results that would justify expanded efforts. We obtained consent from all sample providers.
Overall, we learned that issues of sample procurement need to be overcome to advance our understanding of molecular cancer disparities at the race/ethnicity level.
From the standpoint of race, cancer databases may not be large
For molecular studies, cancer researchers regularly consult with cancer databases (e.g., TCGA). However, these may not be complete. They are curated over time with entries from various studies. Some reports lack transcriptome data (i.e., microarray or next-generation sequencing), others lack or omit certain covariates such as race or clinical outcomes. Recent modes of molecular analysis, such as microbiome data, are infrequently included.
We consulted colon cancer databases through Genomic Data Commons (NIH-NCI, USA) (https://gdc.cancer.gov), a comprehensive data curation site, to see if CRC transcriptome data were available by race. At the time of the manuscript revision (April 5, 2023), CRC data entry by race/ethnicity in the database were as follows: white 4229, not reported 2348, unknown 522, Black or AA 492, Asian 272, other 114, not allowed to collect 67, AI or Alaska native 11, and native Hawaiian or other Pacific Islander 1. The totals were colon, 6940 and rectal, 1116. Among the 11 AI samples, only 2 had transcript profiling data.
The entry numbers themselves indicate disparities. For race/ethnicity groups with small numbers of data entry, solid statistics and model building (machine-learning or otherwise) are difficult. A simple and effective remedy would be to obtain more samples and data entries.
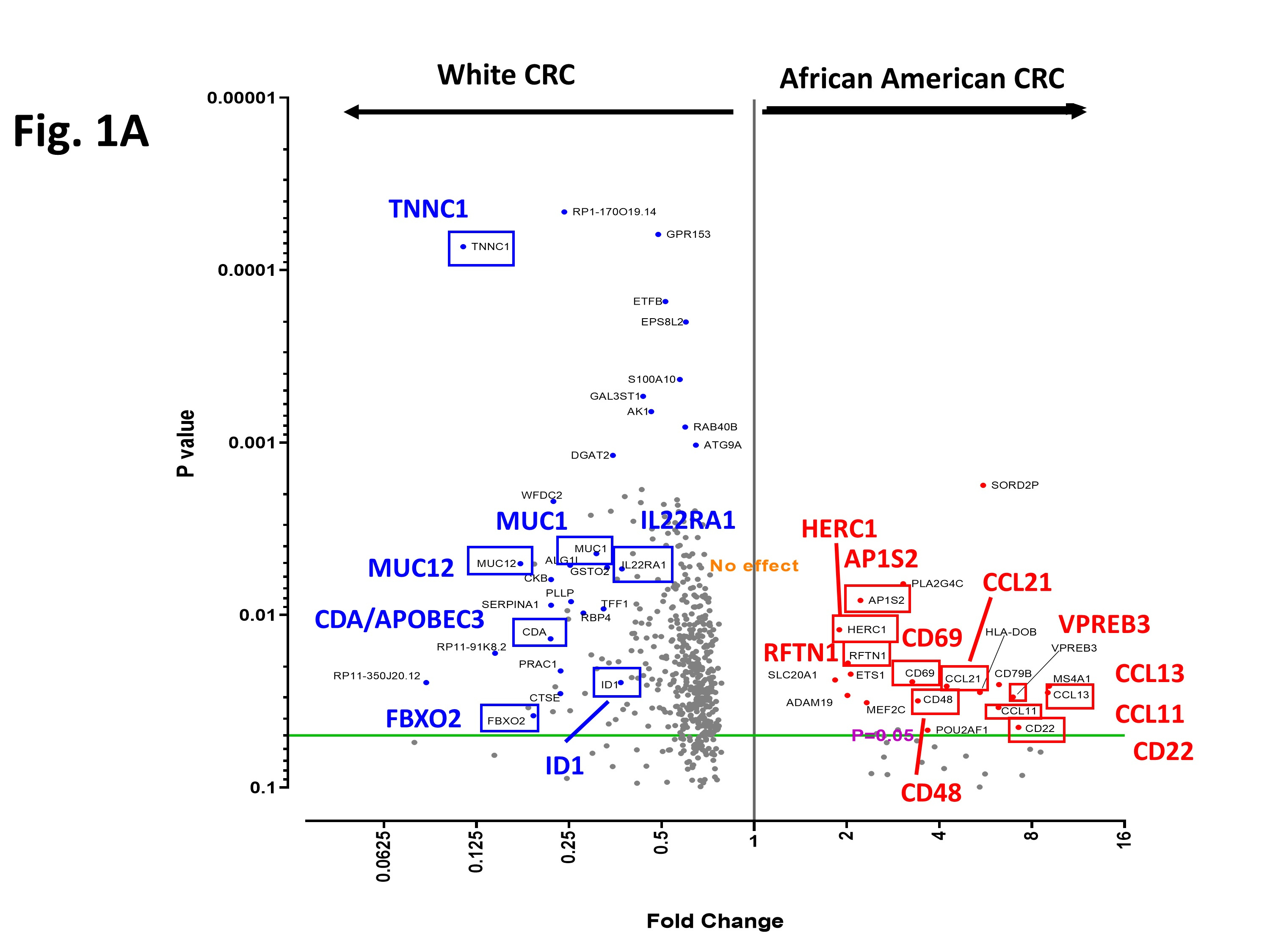
Our results in short
In the manuscript, (quoting the Abstract) “we compared transcriptomic profiles of CRCs of Alabama African Americans, Oklahoma American Indians, and white people from both states. Compared to CRCs of white people, CRCs of AAs showed (a) higher expression of cytokines and vesicle trafficking toward modulated antitumor-immune activity, and (b) lower expression of the ID1/BMP/SMAD axis, IL22RA1, APOBEC3, and Mucins; and AIs had (c) higher expression of PTGS2/COX2 (an NSAID target/pro-oncogenic inflammation) and splicing regulators, and (d) lower tumor suppressor activities (e.g., TOB2, PCGF2, BAP1). Therefore, targeting strategies designed for white CRC patients may be less effective for AAs/AIs.”
Implications in clinical application and drug development
Investigators frequently use differentially expressed genes (DEGs) as rationales to select drug development targets. The present molecular analysis study points out, for the first time, that DEG profiles are different among CRCs from whites, Alabama AAs, and Oklahoma AIs. Differences in DEGs can result in pursuit of drug targets that may be effective for CRCs of white patients but have limited efficacy for Black patients. Thus, our results will raise awareness to race/ethnicity or to community-based DEGs.
In current practice of personalized medicine, clinicians collect tumor tissue or liquid biopsies, then generate reports on mutational profiles of known oncogenes, tumor suppressors, PD1 status and other pathways, and/or tumor mutational burden. Based on the profiles, they devise a treatment strategy. For example, PD1 status justifies use of a PD1/PDL1 blocker and BRCA1 status a PARP inhibitor.
Thus, personalized medicine is practiced with a focus on identified biomarkers (i.e., it is biomarker-driven) and existing, but limited, sets of targeting drugs. If current practice continues to focus on the biomarkers for white Americans, biomarkers prominent in a race/ethnicity-specific manner may not be identified. The present study will help to raise awareness on the need to investigate race/ethnicity-specific biomarkers that can be integrated into personalized medicine.
With identification of sets of race/community-specific/pronounced DEGs, the new biomarkers can be included in clinical cancer analyses and can guide decision-making by clinician-oncologists toward improvements in clinical outcomes.
Conclusions
From the research community and from respected publishers, there is a growing demand for scientific rigor and solid statistical bases for conclusions. Disparities in cancer outcomes among races/ethnicities are known, yet the underlying molecular factors remain to be discovered. The present work will serve as a proof-of-principle of the need for molecular cancer analysis focused on race/ethnicity, so that procurement difficulties will be overcome, and work that is more relevant will follow.
Follow the Topic
-
npj Precision Oncology

An international, peer-reviewed journal committed to publishing cutting-edge scientific research in all aspects of precision oncology from basic science to translational applications to clinical medicine.
Related Collections
With Collections, you can get published faster and increase your visibility.
AI Approaches in Drug Design
Publishing Model: Open Access
Deadline: Mar 31, 2026
Genomic Instability
Publishing Model: Open Access
Deadline: Mar 24, 2026

Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in