Cost effectiveness of a novel SwaRSA Strategy to reduce acute exacerbations of COPD
Published in Neuroscience, Protocols & Methods, and General & Internal Medicine
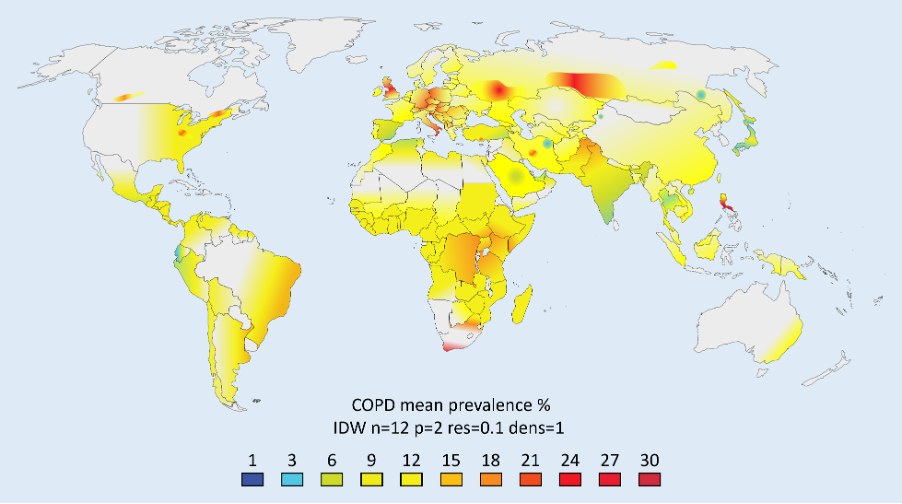
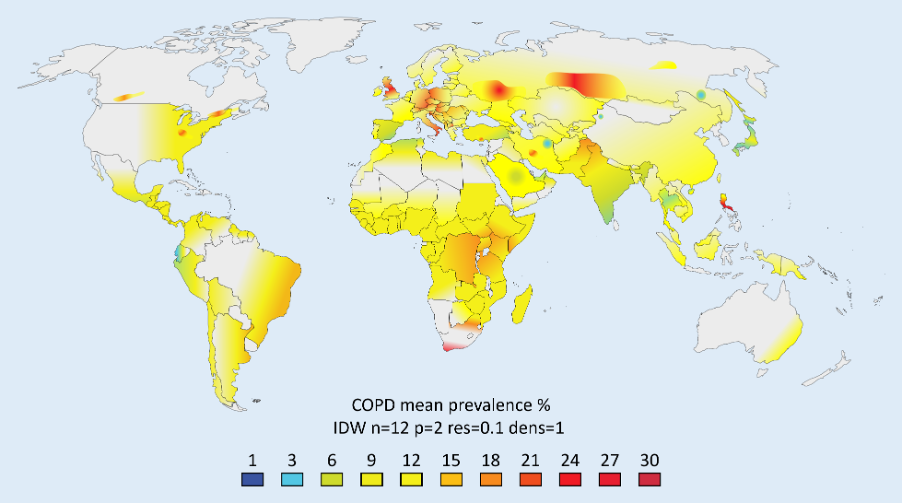
The paper discusses the significant economic burden of Chronic Obstructive Pulmonary Disease (COPD) and the potential cost savings from reducing COPD exacerbations. A decision analytic model that evaluates the cost-effectiveness of a Swallowing and Respiratory Sensation Assessment (SwaRSA) strategy, involving swallowing and respiratory sensation assessment tests and subsequent swallowing rehabilitation, is presented to reduce COPD exacerbations. The model suggests that self-assessment with the Eating Assessment Tool (EAT-10) and subsequent intervention is a highly cost-effective option compared to no-SwaRSA.
Key Points: Novel SwaRSA Decision Analytic Model; Epiu I. et al 2025 https://pubmed.ncbi.nlm.nih.gov/40200355/
Economic Burden of COPD
- COPD represents a considerable economic burden globally, with an estimated cost of US$ 2.1 trillion.
- Annual COPD costs in the USA are expected to increase to 40 billion USD per year.
- Australia spent about AUD$ 831.6 million in 2020-21 on the management of COPD, with over half of this cost for hospital care.
Potential for Cost Savings
- A significant portion of the COPD management cost could be avoided by reducing exacerbations.
Cost-Effectiveness of SwaRSA Strategy
- The decision analytic model assessed the cost-effectiveness of a Swallowing and Respiratory Sensation Assessment (SwaRSA) strategy, which involved swallowing and respiratory sensation assessment tests and subsequent swallowing rehabilitation.
- Three individual testing strategies within the SwaRSA approach were found to be cost-effective, with incremental cost-effectiveness ratios per QALY ranging from $27,000 to $37,000 AUD.
- The EAT-10 and the tongue strength were the two dominant options on the cost-effectiveness frontier.
- The model results were robust to variations in one-way and probabilistic sensitivity analyses, and the self-assessment with the EAT-10 and subsequent intervention was highly cost-effective relative to no-SwaRSA.
Here are the key implications of the findings for healthcare policy regarding COPD management:
-
The high economic burden of COPD, estimated at over $2 trillion globally and $40 billion annually in the US, highlights the need for more effective and cost-efficient management strategies.
-
Novel finding that a significant portion of COPD costs could be avoided by reducing exacerbations suggests that interventions targeting exacerbation prevention should be a priority for policymakers.
-
The high prevalence of swallowing difficulties (dysphagia) among COPD patients, affecting up to 56% of hospitalized patients, suggests that screening and management of swallowing disorders should be integrated into standard COPD care.
-
This cost-effectiveness analysis of the SwaRSA strategy, which includes swallowing and respiratory sensation assessment tests followed by swallowing rehabilitation, provides strong evidence that such an approach can be a highly cost-effective way to reduce COPD exacerbations and associated costs.
-
Further research may be needed to validate these findings in different healthcare settings and populations, but the current evidence suggests that integrating swallowing assessment and rehabilitation into COPD management should be a priority for healthcare policy
Follow the Topic
-
BMC Pulmonary Medicine

This journal is an open access, peer-reviewed journal that considers articles on all aspects of the prevention, diagnosis and management of pulmonary and associated disorders, as well as related molecular genetics, pathophysiology, and epidemiology.
🔍 Ask the Editor – Clinical medicine, Respiratory physiology, and Cardiology
I’m excited to connect with a global network of specialists through the Research Communities – how will you get involved?
Continue reading announcementRelated Collections
With Collections, you can get published faster and increase your visibility.
Cancer and the lung
BMC Pulmonary Medicine is calling for submissions to our Collection on Cancer and the lung. Lung cancer remains one of the most prevalent forms of cancer worldwide, presenting unique challenges in both diagnosis and treatment. The complexity of lung cancer is exacerbated by the interplay between pulmonary conditions and various risk factors, including smoking, environmental exposures, and genetic predispositions. With advances in research, there is a growing understanding of the molecular mechanisms intertwined with lung cancer development and progression. The need for innovative approaches to diagnosis and treatment, as well as effective management strategies for patients, is more critical than ever in the fight against this devastating disease.
Research in the field of lung cancer has witnessed significant progress, particularly with the advent of targeted therapies and immunotherapies that have transformed treatment paradigms. As we gain more insight into the biology of lung cancer, we are better equipped to tailor therapeutic strategies that not only improve survival rates but also enhance the quality of life for patients. Understanding the role of lung cancer in the context of immunosuppression and infection opens new avenues for enhancing patient outcomes, especially in those with comorbidities. Potential research topics can include but are not limited to:
•Mechanisms of lung cancer development
•Innovations in lung cancer diagnosis
•Immunotherapy and lung cancer treatments
•Impact of lung infections in cancer patients
•Chemotherapy and its effects on lung health
This Collection supports and amplifies research related to SDG 3: Good Health and Well-being.
Publishing Model: Open Access
Deadline: Mar 11, 2026



Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in