Exploring co-design practices in digital health interventions
Published in Bioengineering & Biotechnology and Public Health

Digital health interventions aim to improve patient health and health care delivery. These interventions are delivered through digital tools including mobile phones, tablets and wearable devices which collect, store and analyze health information and have been shown to positively improve changes in disease self-management, clinical outcomes and quality of life across diverse populations of patients. Despite this success, there are still challenges with these interventions including a lack of adoption by patients and caregivers and poor integration into routine clinical care.
Design and development of these interventions is a complex process, and the lack of meaningful end-user involvement is a key contributor to limited intervention use by end-users. Co-design, a collective creative approach where varied stakeholders including patients, clinicians and policy makers are actively involved in the development, design and implementation of interventions has been suggested to address this pitfall. However, co-design strategies are inconsistently implemented in the development of digital health interventions, and there is currently no clear understanding or guideline on how best to conduct a co-design of a digital health intervention.
Our interdisciplinary and international research group of clinicians (specializing in a diverse range of patients from pediatric to geriatrics), researchers and digital health experts from the University of Toronto and the University of Manchester, has a keen interest in addressing this gap in standardized use. Our goal is to understand how co-design of digital health interventions can be improved, standardized, and made more equitable to ensure patients and caregivers across health conditions receive high quality interventions tailored to the population’s needs, attitudes and values. Our first step was to synthesize the literature focused on co-design in digital health. Specifically, we asked the following question: what is known about the practical methods to conduct co-design of digital health interventions (including setting, population, intervention details, session length, co-design strategy) and the breadth and depth of end-user involvement in the process?
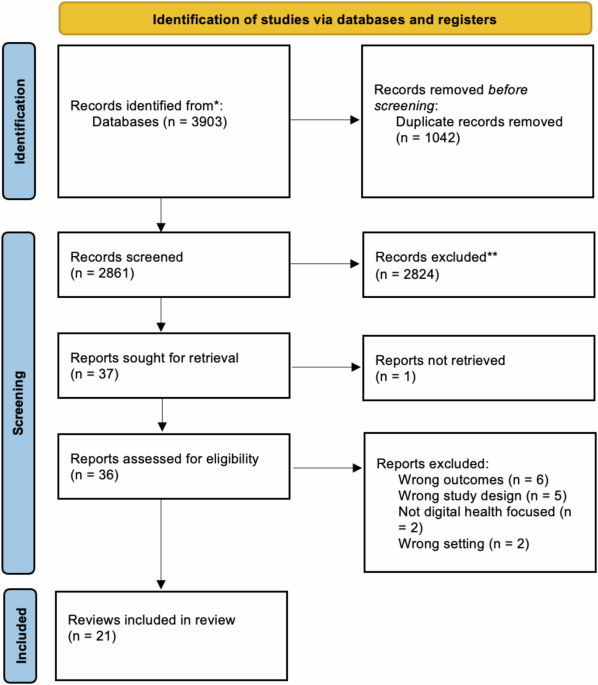
To answer this question, we completed a systematic review of reviews. We searched five databases from inception to March 8th, 2023. Reviews were included if they focused on co-design of an intervention aimed at managing an acute or chronic health condition or promoting healthy lifestyle habits and if end-users of the intervention were patients or the public. We also assessed the quality of each review using the A Measurement Tool to Assess Systematic Reviews 2 (AMSTAR-2).
Studies. In total, we identified 21 reviews which met our inclusion criteria. Most were published in developed countries including Australia, the United Kingdom, Canada and the United States and published in 2022, 2020 and 2019. Most commonly, reviews focused on digital, mobile or electronic health interventions and were targeted towards individuals with chronic conditions. A wide range of terminology was used to describe co-design including participatory design and human-centered development. Overall, all reviews were classified as critically low quality using the AMSTAR-2 tool.
Participants. Patients, caregivers, healthcare professionals, teachers and behaviour specialists participated in co-design activities. Unfortunately, demographics including specific age ranges, race and ethnicities and sex or gender were infrequently reported by reviews.
Activities. Surveys, focus groups and interviews were the most frequently used type of co-design activities. The specific location in which activities took place including online, in community centres or at hospitals was infrequently reported by reviews. This inconsistent reporting was also noted in reporting pertaining to the duration and frequency of the sessions. However, twelve of the reviews provided details on the aspects of the intervention that participants helped co-design including illustrations, content and animations.
Evaluation. Only a small number of reviews reported on how participant’s felt regarding participating in co-design activities and although they reported overall high levels of satisfaction; most of the reviews emphasized that this was infrequently assessed in the studies they identified.
Challenges and Equity. Frequently cited challenges to co-design included power imbalances between researchers and participants, financial constraints, difficulty recruiting participants and group think. Identified strategies to address these include building relationships and trust, empowering the end-user and establishing values and interest. Eight reviews reported on accessibility and equity including the power of involving cultural advisors in co-design sessions and using a proactive outreach approach to recruit vulnerable populations.
Our review highlights the inconsistent reporting of co-design activities in digital health and emphasizes the need to create standardized guidelines for reporting co-design methodologies to direct the process, with emphasis on guidance that ensures engaging and effective co-design in particular populations and health conditions.
To address this need, we suggest a series of next steps, which we hope to achieve in our future collaborative work, to standardize the co-design process. These steps include standardizing the terminology used in co-design, determining a set of minimally required participant sociodemographic data and reporting on co-design activity details, establishing clear success metrics using both qualitative and quantitative measures and surveying participants prior to sessions to identify population specific challenges and accessibility concerns. Ultimately, to be truly emblematic of co-design principles, these guidelines should be co-created with patients and caregivers and include meaningful involvement of healthcare professionals to enhance capacity to create clinically relevant digital health tools. Suck work has the potential to ensure co-design as a principle in the development of effective and sustainable future digital health interventions.
Follow the Topic
-
npj Digital Medicine

An online open-access journal dedicated to publishing research in all aspects of digital medicine, including the clinical application and implementation of digital and mobile technologies, virtual healthcare, and novel applications of artificial intelligence and informatics.
Related Collections
With Collections, you can get published faster and increase your visibility.
Evaluating the Real-World Clinical Performance of AI
Publishing Model: Open Access
Deadline: Jun 03, 2026
Impact of Agentic AI on Care Delivery
Publishing Model: Open Access
Deadline: Jul 12, 2026



Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in