Fat and liver health: the view from LXRalpha
Published in Biomedical Research
The thinking behind this paper started about 7 years ago. The lab had some experience, through the study of PPARγ (in collaboration with Krish Chatterjee) of how novel insights into the biology of nuclear receptors could be obtained by studying humans carrying dominant negative mutations. We began to wonder whether other nuclear receptors might yield to similar approaches. Classically, humans with such mutations had been identified in the process of clinical evaluation of patients or by research-based sequencing of disease cohorts. However, the advent of large population biobanks with detailed phenotypic information has facilitated a ‘genotype-first’ approach where sequencing data can be queried for proven or predicted damaging mutations in genes of interest. Existing phenotypic information can then be interrogated for any significant associations. We first explored this ‘reverse-genetics’ approach in humans in a study of PPARα undertaken by a talented clinical endocrinologist working in the lab (Dr Audrey Melvin, manuscript in preparation). Those studies played a key role in informing our work on another nuclear receptor – LXRα - a cholesterol sensing nuclear receptor highly expressed in the liver and adipose tissue. Studies in cells and mice previously demonstrated a key role for this molecule in regulation of cellular cholesterol homeostasis and it is also known to potently activate lipogenesis. However, the significance of these findings to human health was less clear.
What we found
To provide insight into the role of LXRα in human cardiometabolic health we characterised >60 mutations in LXRa that were found in participants of either UK biobank or a cohort study in East Anglia, the Fenland study. Greater than 1 in 500 people carry a mutation in one copy of the LXRα gene causing substantial impairment in the receptor when assessed in vitro. On average, these people have lower serum triglycerides consistent with loss of the known lipogenic effects of LXRα as well as higher HDL levels. The effect of LXRα impairment on HDL cholesterol levels exemplifies the importance of translational studies in humans; LXR agonism upregulates HDL cholesterol in mice wheras we find an inverse relationship between LXRa activity and HDL cholesterol and small RCTs of LXR-agonists in humans find similar results. Such discrepancy is likely due to the presence of CETP in humans but not rodents which is induced by LXRα and reduces cholesterol in HDL by exchanging it for triglycerides from triglyceride rich lipoproteins. We were also pleased to see a nice dose-response relationship between the degree of functional impairment of the mutant and HDL cholesterol levels reassuring us that differences in functional activity were reflected in real in vivo biology in humans. A more surprising finding was that these people had elevated liver enzymes suggestive of subclinical hepatotoxicity despite harbouring a defect in a key lipogenic nuclear receptor.
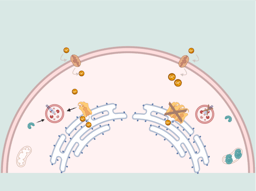
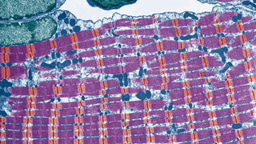
To explore the role of LXRα in liver health in more detail we generated a knock-in mouse model carrying one the most damaging mutations we characterised (p.W441R) which exhibits impaired transactivation function and is strongly dominant negative. When subject to dietary cholesterol challenge, these mice accumulate cholesterol in their livers and develop severe fibrotic liver injury within a matter of weeks. Strikingly, this occurs despite markedly suppressed liver triglyceride levels and in the absence of visible steatosis. The observed liver injury is dependent on a direct impairment in hepatocyte LXR-signalling as liver injury could be prevented by expressing wildtype LXRα in hepatocytes alone. In collaboration with Peter Tontonoz and Alessandra Ferrari we studied LXRα-knockout mice which lack LXRα activity but do not possess the repressive actions of a dominant negative LXRα isoform. These mice accumulate cholesterol in liver to levels similar to the knock-in mice but do not have changes in hepatic triglyceride levels and develop much milder liver injury.
Excess cholesterol can crystallise and provoke an immune response via activation of the inflammasome. Therefore, we conducted polarised microscopy to assess for cholesterol crystal accumulation. Cholesterol crystals were not detected in wildtype mice fed a western diet for 8 weeks but were abundant in knock-in mice. Consistent with inflammasome activation IL-1b was markedly upregulated in knock-in mice. Interestingly, LXRα -knockout mice which develop much milder liver injury do develop cholesterol crystals in the liver, but this is restricted to areas where steatosis is limited raising the intriguing possibility that lipogenesis and hepatic lipid droplet formation may somehow protect against cholesterol crystallisation.
Why is it important?
Our work has some important translational implications. As hepatic triglyceride accumulation is a defining feature of steatotic liver disease it is not surprising that many have proposed inhibition of hepatic lipogenesis as a potential therapeutic strategy. Inverse agonists to LXR have been developed and are currently being tested in for use in MASLD and severe hypertriglyceridemia in early phase clinical trials. Our work provides evidence that impaired LXR-signalling is likely to be hepatotoxic, a finding which raises a safety flag over any research programme examining the effects of LXRα antagonism or inverse agonism in humans.
There is increasing interest in the role of cholesterol accumulation in the pathogenesis of metabolic dysfunction associated steatotic liver disease (MASLD) but evidence supporting a role for cholesterol in MASLD has been limited either to observational studies, which do not permit clear attribution of causality or to studies using genetic instruments, which may be confounded by parallel effects of genetic variants on hepatic cholesterol and triglyceride content. Our study of LXRα provides direct evidence of a causal effect of liver cholesterol accumulation on hepatoxicity. Notably, we also found that carriers appeared at greater risk of clinically diagnosed alcohol-related liver disease, but this was based on a small number of affected carriers and needs to be re-tested in large case-control cohorts.
It should be noted that while mice carrying a dominant-negative mutation in homozygosity had much more severe liver injury than their knockout counterparts, there was no evidence of a stronger effect of heterozygous carriage of a dominant negative mutation on liver enzymes in UKBB participants than carriage of a simple loss of function mutation. This likely relates to statistical power: the dominant negative mutations we discovered mostly exhibited only mild dominant negative actions in vitro and were much rarer than simple loss of function mutations.
Follow the Topic
-
Nature Metabolism

This journal publishes work from across all fields of metabolism research that significantly advances our understanding of metabolic and homeostatic processes in a cellular or broader physiological context, from fundamental cell biology to basic biomedical and translational research.


Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in