How a High-Performance Polymer Is Changing the Future of Orthopaedic Implants
Behind the Story:
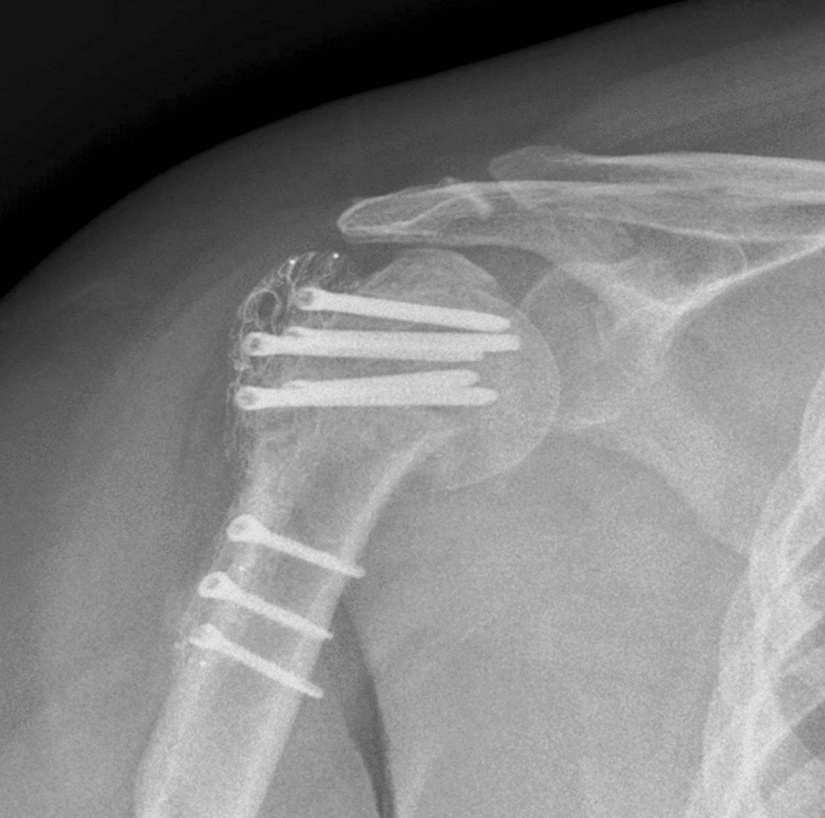
When we think about joint replacements or fracture fixation in orthopaedics, most people picture shiny metallic implants — often made of stainless steel, titanium alloys, or cobalt-chromium. These metals have been the gold standard for decades because they’re strong, durable, and well-tested. But metals also come with limitations: they’re much stiffer than bone, can cause imaging artefacts on X-rays and MRIs, and in rare cases, may trigger allergic reactions.
This review is not just a technical summary. It tells a story about how materials science, engineering, and clinical practice are converging to rethink what implants can be — and what they should be — for patients and surgeons alike.
Why Does Implant Material Matter So Much?
Imagine replacing a damaged knee joint. The implant you receive has to do more than just fill a space — it has to withstand years of repeated stress, support your body weight, and integrate with your bones and tissues without causing harm. Traditional metals do this fairly well, but they aren’t perfect:
-
Mismatch in stiffness: Metals are much stiffer than bone. Bone, in contrast, has a lower elastic modulus — a measure of how much it bends under stress. Because metals are so rigid, they can unintentionally “shield” nearby bone from stress. This can lead to bone weakening or resorption over time.
-
Imaging challenges: Metallic implants show up brightly on X-rays and can create visual artefacts on CT and MRI scans, sometimes obscuring key details surgeons want to see post-operation.
-
Allergic responses: While rare, some patients may react to metal ions released over time.
These limitations prompted researchers and engineers to explore new materials that combine mechanical strength with biological friendliness — and that’s where PEEK comes in.
Introducing PEEK — A Smart, Bone-Friendly Material
Polyetheretherketone, or PEEK, is a specialized polymer that has been gaining attention in orthopaedics for several reasons:
-
Elasticity similar to bone: PEEK has an elastic modulus much closer to human cortical bone than metals do. This helps reduce the phenomenon of stress shielding and may help preserve bone health around the implant.
-
Radiolucency: Unlike metals, PEEK doesn’t block X-rays or create imaging artefacts. This allows for clearer visualization of the bone-implant interface, improving surgeons’ ability to assess healing and detect complications early.
-
Biocompatibility: PEEK doesn’t release metal ions and carries negligible risk of allergic reactions. Some studies suggest its wear particles provoke a milder inflammatory response than particles from metals or polyethylene, which could have implications for long-term implant health.
But There’s a Catch: The Surface Matters
While PEEK has many ideal properties, its surface — in its native form — is biologically inert. Bone cells don’t naturally cling to or grow into it as readily as they do with metal surfaces. That’s a big obstacle if you want the implant to integrate with the body rather than just sit there.
To overcome this, researchers are exploring surface modification techniques such as:
-
Nano-texturing: Creating microscopic grooves or patterns that encourage bone cells to attach and grow.
-
Bioactive coatings: Applying layers of substances like hydroxyapatite — a mineral naturally found in bone — to make the surface more inviting for bone attachment.
-
Antibacterial additives: Exploring coatings that may reduce infection risk.
These innovations aim to give PEEK implants the best of both worlds: material compatibility with bone and biological integration that supports long-term stability.
How Is PEEK Being Used Today?
PEEK is already being tested in a range of orthopaedic applications:
Joint Replacements (Arthroplasty)
In knee and hip replacement surgery, PEEK components — either alone or reinforced with carbon fibres — have shown promising early results:
-
In some knee replacement studies, PEEK components performed just as well as traditional metal implants in terms of pain relief, function, and early mechanical performance.
-
The radiolucency of PEEK offers a clear advantage for post-surgical imaging, enabling surgeons to monitor healing without the visual noise of metal artefacts.
However, long-term data are still limited, especially for high-load scenarios like hips, where wear resistance and implant survival over decades are critical.
Other Orthopaedic Uses
Outside of joint replacements, PEEK plates are being explored for fracture fixation, where they may allow earlier weight bearing and faster rehabilitation with lower hardware removal rates. PEEK spacers and cages are also used in spine surgery with good early outcomes.
Challenges on the Path to Widespread Use
PEEK isn’t perfect — yet. The technology is still evolving, and there are real challenges that researchers and clinicians are working to address:
-
Long-term clinical evidence: Most studies to date follow patients for only a few years. Large-scale, long-term trials and registry data are needed to determine how PEEK implants hold up over a patient’s lifetime.
-
Manufacturing complexity and cost: PEEK’s processing requirements — especially for advanced surface modifications — are more demanding and expensive than for metals, which may limit access and adoption.
-
Biological integration: While surface treatments help, achieving reliable and predictable bone in growth remains a key area of ongoing innovation.
Looking Ahead: What This Means for Patients and Clinicians
The story of PEEK in orthopaedics is one of promise and ongoing discovery. It represents a shift from thinking of implants as just strong and durable to thinking of them as biomechanically smart and biologically compatible.
For patients, this could mean:
-
Better long-term bone health around implants
-
Fewer imaging limitations
-
Lower risk of metal allergies
For clinicians and researchers, it opens up a wide field of innovation — from materials science to personalised implant design.
Conclusion: Towards a New Chapter in Implant Materials
Materials like PEEK are at the forefront of a new chapter in orthopaedic surgery — one where implants no longer just replace what’s broken but work harmoniously with the body they support. Our review highlights the remarkable strides made so far and the exciting paths still ahead, underscoring both the current evidence and the research questions that future studies must answer.
This isn’t the end of the story — but it’s a promising beginning.
Follow the Topic
-
European Journal of Orthopaedic Surgery & Traumatology

The European Journal of Orthopaedic Surgery and Traumatology is focused on publishing high-quality, clinically relevant orthopedic research from around the world.
Related Collections
With Collections, you can get published faster and increase your visibility.
RECENT ORTHOPAEDIC TRENDS IN ASIA PACIFIC
Publishing Model: Hybrid
Deadline: Ongoing
Global Spine Perspectives: Quality, Innovation, and Collaboration
Publishing Model: Hybrid
Deadline: Ongoing
Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in