Very old patients need palliative care,not intensive care - an empirical and normative analysis
Published in Mechanical Engineering and Philosophy & Religion
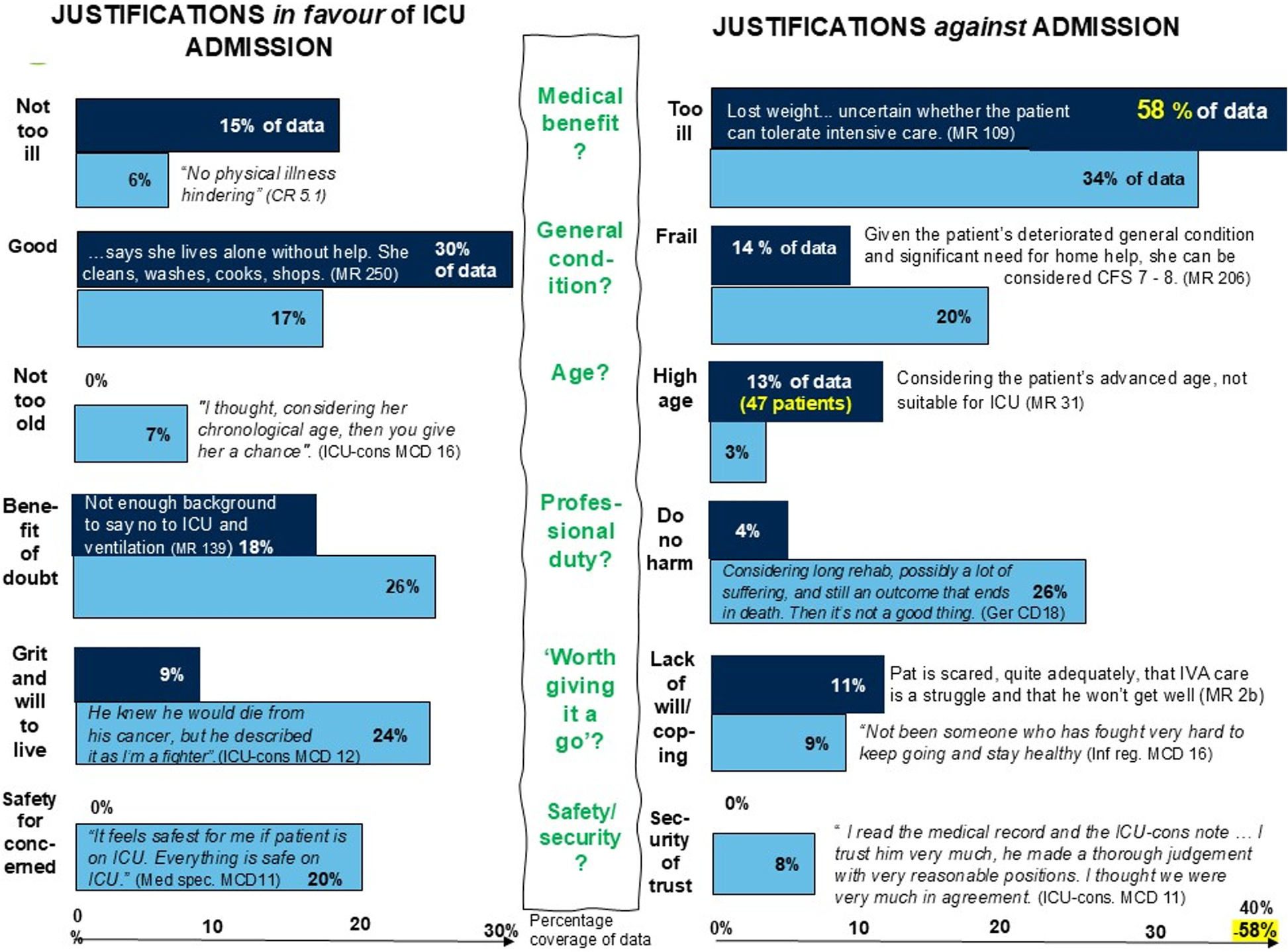
We found clear and consistent evidence – both quantitative and qualitative – that high chronological age is a key factor against ICU admission. Among all the variables we compared, only being 80 years or older clearly stood out as linked to not being admitted to intensive care.
Across every data source, high age kept reappearing as a justification for non-admission. In medical records, “considering age” was mentioned again and again. In the COVID Rounds, Moral Case Deliberations (structured reflections on ethically complex patient cases), and follow-up interviews, the phrase “very old” was used repeatedly when decisions were discussed.
Another powerful justification across all data was about not harming the patient. This included avoiding unworthy suffering, not subjecting patients to what was described as torture when ICU care offered no benefit and recognising ventilator treatment as risky. For patients over 80, ICU care was often described as unacceptable; at 90, death was seen as a natural event. One ICU consultant put it poignantly:
“Ninety feels like, if you’ve had a good life and you’re spry and healthy ... if you die suddenly, then it’s expected. And better than dragging to the ICU and tormenting the person.”
Interestingly, few justifications were directly linked to the pandemic. The patterns we found mirror those from pre-COVID studies, suggesting that what we captured ordinary clinical decision-making, not crisis-specific thinking.
Normative discussion
When discussing chronological age as a factor, our findings align with two key ethical principles: non-maleficence and justice.
Non-maleficence implies here sparing patients from unnecessary suffering and loss of dignity. Distributive justice connects with the ICU prioritisation literature, which tends to exclude patients “with a fuller lifecycle.” In intensive care, defining what counts as a need becomes crucial.
According to Swedish legislation, healthcare needs are defined by both the severity of a condition and the potential benefit of treatment. For very old patients, with higher ICU mortality and poorer recovery rates, the potential benefit is often limited. From this perspective, ICU care may not truly meet very old patients’ needs.
Following the legal principle of Need and Solidarity, treatment should only be prioritised when there is potential for benefit. Our results therefore suggest that many very old patients are better served by palliative rather than intensive care.
A call for courage and clarity
We believe it is time for a national – and perhaps international – guiding policy on triage systems for very old patients in everyday care. Such a policy should be developed with courage and transparency, openly supporting a palliative approach for the very old.
Follow the Topic
-
BMC Medical Ethics

This journal is an open access journal publishing original peer-reviewed research articles in relation to the ethical aspects of biomedical research and clinical practice, including professional choices and conduct, medical technologies, healthcare systems and health policies.
Related Collections
With Collections, you can get published faster and increase your visibility.
Moral status and ethical implications of abortion
The moral status and ethical implications surrounding abortion have been subjects of intense debate across various cultural, religious, and philosophical contexts. Addressing the ethical dimensions of abortion is essential for developing frameworks that support informed decision-making and respect for diverse beliefs. Recent advancements in bioethics have fostered a more nuanced understanding of reproductive choice, leading to improved policies and practices that prioritize women's health and autonomy. Additionally, the societal impact of landmark legal cases, such as Roe v. Wade, continues to shape the discourse on reproductive rights, emphasizing the importance of ongoing examination of ethical principles in this arena.
BMC Medical Ethics is calling for submissions to our Collection on Moral status and ethical implications of abortion. This Collection seeks to explore the complexities of abortion ethics, including questions of maternal autonomy, reproductive justice, and the competing moral frameworks that inform individuals’ and societies’ views on this critical issue. Key topics of interest for submission include, but are not limited to:
Maternal autonomy in reproductive decision-making
Reproductive justice and abortion rights
Moral conflict and abortion ethics
Religious perspectives on abortion
Societal impact of Roe v. Wade
All manuscripts submitted to this journal, including those submitted to collections and special issues, are assessed in line with our editorial policies and the journal’s peer review process. Reviewers and editors are required to declare competing interests and can be excluded from the peer review process if a competing interest exists.
Publishing Model: Open Access
Deadline: Apr 02, 2026
Global health equity and ethics
BMC Medical Ethics invites submissions to our new Collection, Global health equity and ethics. The concept of global health equity encompasses the moral principles that guide health policies and practices aimed at reducing disparities in healthcare access and outcomes among different populations. As the world becomes increasingly interconnected, ethical considerations surrounding health equity are more critical than ever.
Promoting health equity is an ethical imperative in public health. As social determinants continue to drive disparities, public health ethics and ethical advocacy are essential to ensuring that policies and interventions are not only effective but also just. We encourage research that confronts these ethical challenges and supports a more equitable healthcare landscape.
This Collection welcomes submissions that explore the ethical dimensions of health equity, examining the systemic barriers that marginalized populations face and how these barriers can be dismantled to promote equitable healthcare for all. Key topics of interest for submission include, but are not limited to:
Ethical considerations in healthcare access
Addressing global disparities in health outcomes
Health justice and marginalized populations
Social determinants of health and health inequities
Policy implications for equitable healthcare
This Collection supports and amplifies research related to SDG 3: Good Health and Well-Being, SDG 10: Reduced Inequalities, and SDG 16: Peace, Justice and Strong Institutions.
All manuscripts submitted to this journal, including those submitted to collections and special issues, are assessed in line with our editorial policies and the journal’s peer review process. Reviewers and editors are required to declare competing interests and can be excluded from the peer review process if a competing interest exists.
Publishing Model: Open Access
Deadline: Jun 30, 2026


Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in