Fine Needle Aspiration Cytology (FNAC): Technique, Applications, and Standardized Reporting Across Anatomical Sites
Published in General & Internal Medicine
Fine Needle Aspiration Cytology (FNAC) is a cornerstone of modern diagnostic pathology, particularly valuable in resource-limited settings and early triage of lesions. It is a minimally invasive, safe, and cost-effective procedure that allows rapid evaluation of superficial and deep-seated masses. FNAC has gained prominence in the diagnostic algorithm of various diseases, especially those involving the thyroid, salivary glands, lymph nodes, breast, and soft tissues. With proper technique and interpretation, FNAC can differentiate between benign, reactive, infectious, and malignant conditions with high accuracy.
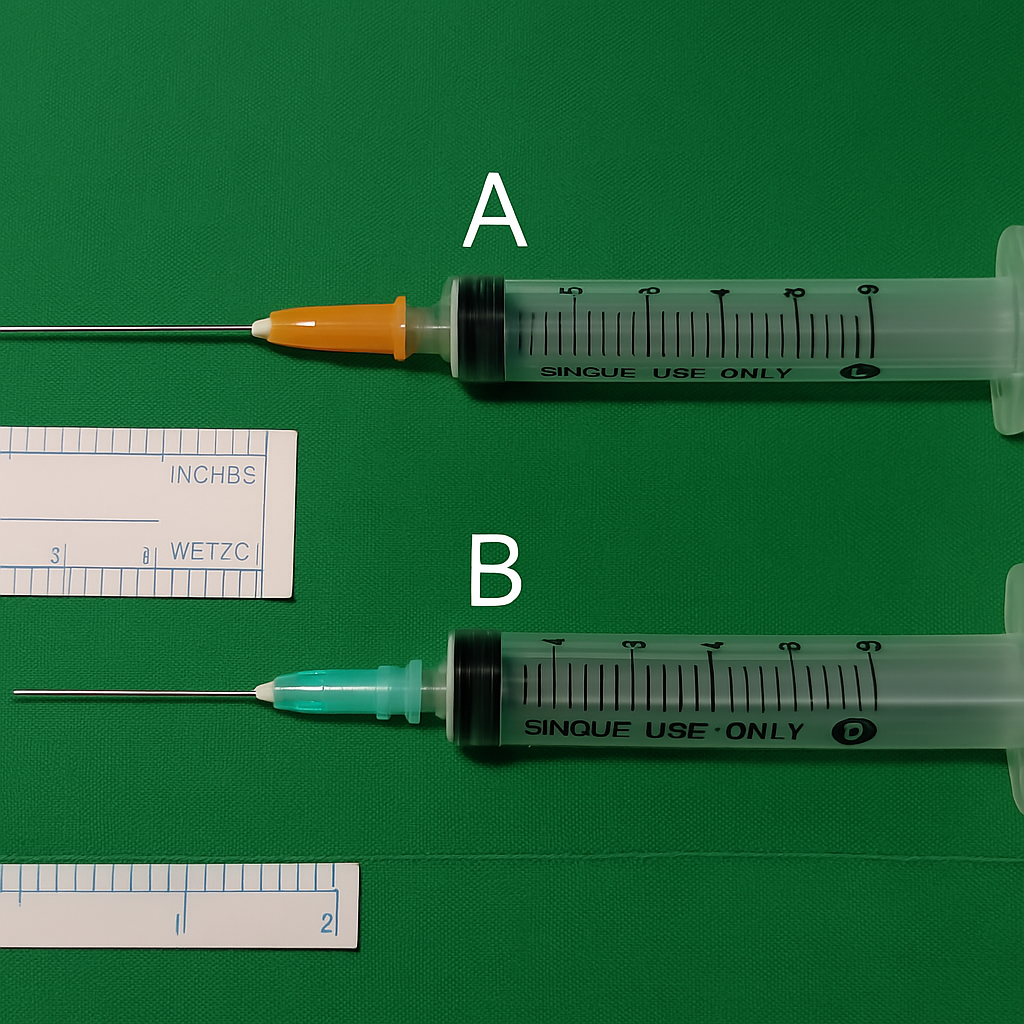
FNAC is usually performed using a 22–27 gauge needle attached to a 10 mL disposable syringe. The procedure can be done by palpation for accessible lesions or under image guidance, such as ultrasound, CT, or endoscopic visualisation for deeper or non-palpable sites. Image-guided FNAC is particularly essential in evaluating thyroid nodules, deep lymphadenopathy, parotid gland masses, or retroperitoneal lesions. Both aspiration and non-aspiration (capillary action) techniques are used depending on the lesion type and vascularity. The material obtained is expelled onto glass slides, immediately fixed in ethanol for Papanicolaou staining or air-dried for Giemsa or Romanowsky staining. In cases requiring further workup, FNAC samples may also be processed for ancillary techniques including immunocytochemistry (ICC), flow cytometry, fluorescence in situ hybridisation (FISH), and molecular assays such as PCR or NGS.
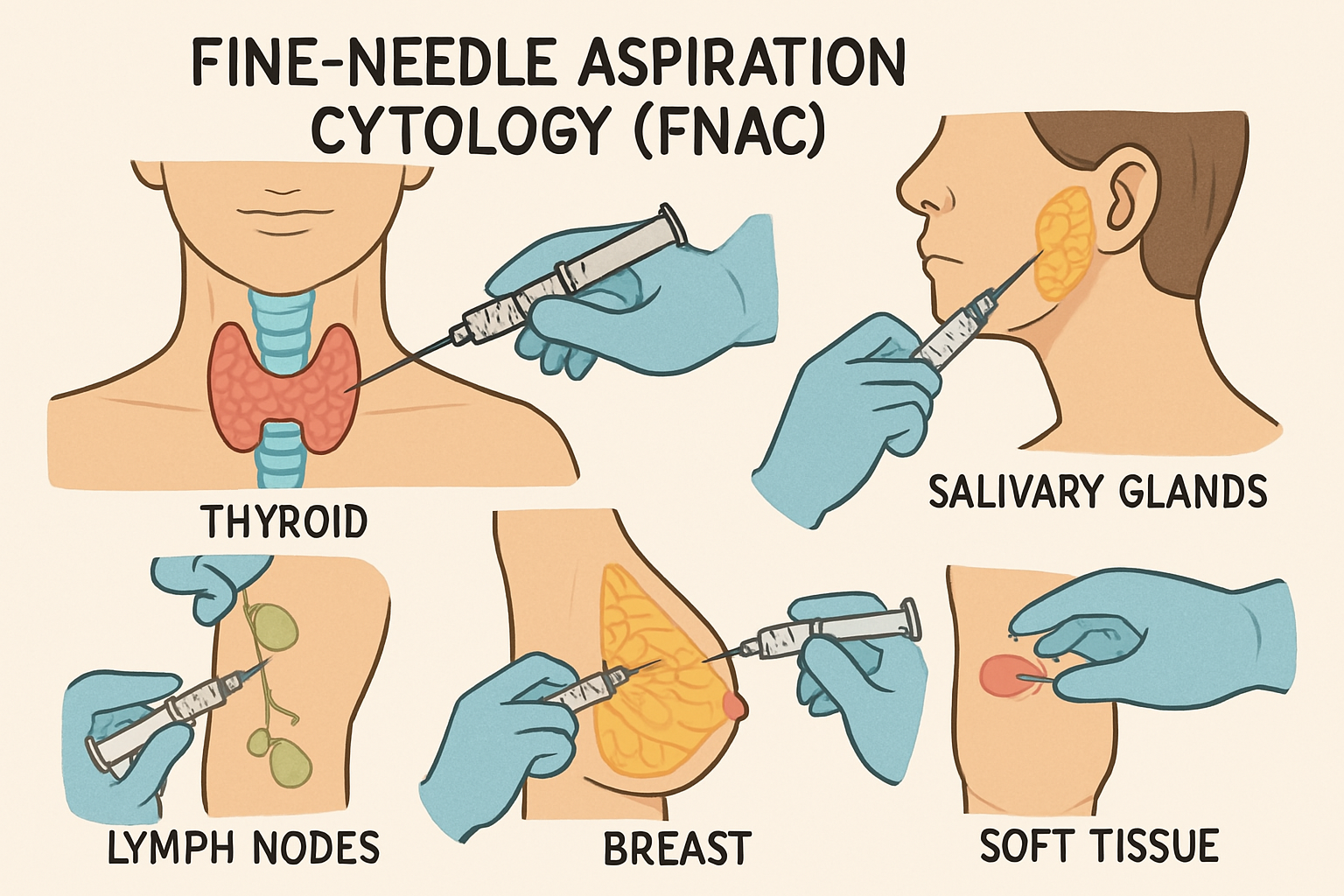
The most common anatomical sites for FNAC include the thyroid gland, where it is essential for evaluating nodules under The Bethesda System for Reporting Thyroid Cytopathology (TBSRTC); salivary glands, following The Milan System; and lymph nodes, particularly in infectious diseases, metastasis, or lymphoma evaluation, where the Sydney System is useful. FNAC of the breast, guided by the IAC Yokohama System, provides a structured categorisation of breast lesions. It is also increasingly used for submandibular, oral, and oropharyngeal swellings, aiding the differential diagnosis of granulomatous diseases like tuberculosis, reactive lymphoid hyperplasia, or metastatic squamous cell carcinoma. In soft tissue and pediatric tumours, FNAC aids in identifying small round cell tumours, sarcomas, and atypical lesions.
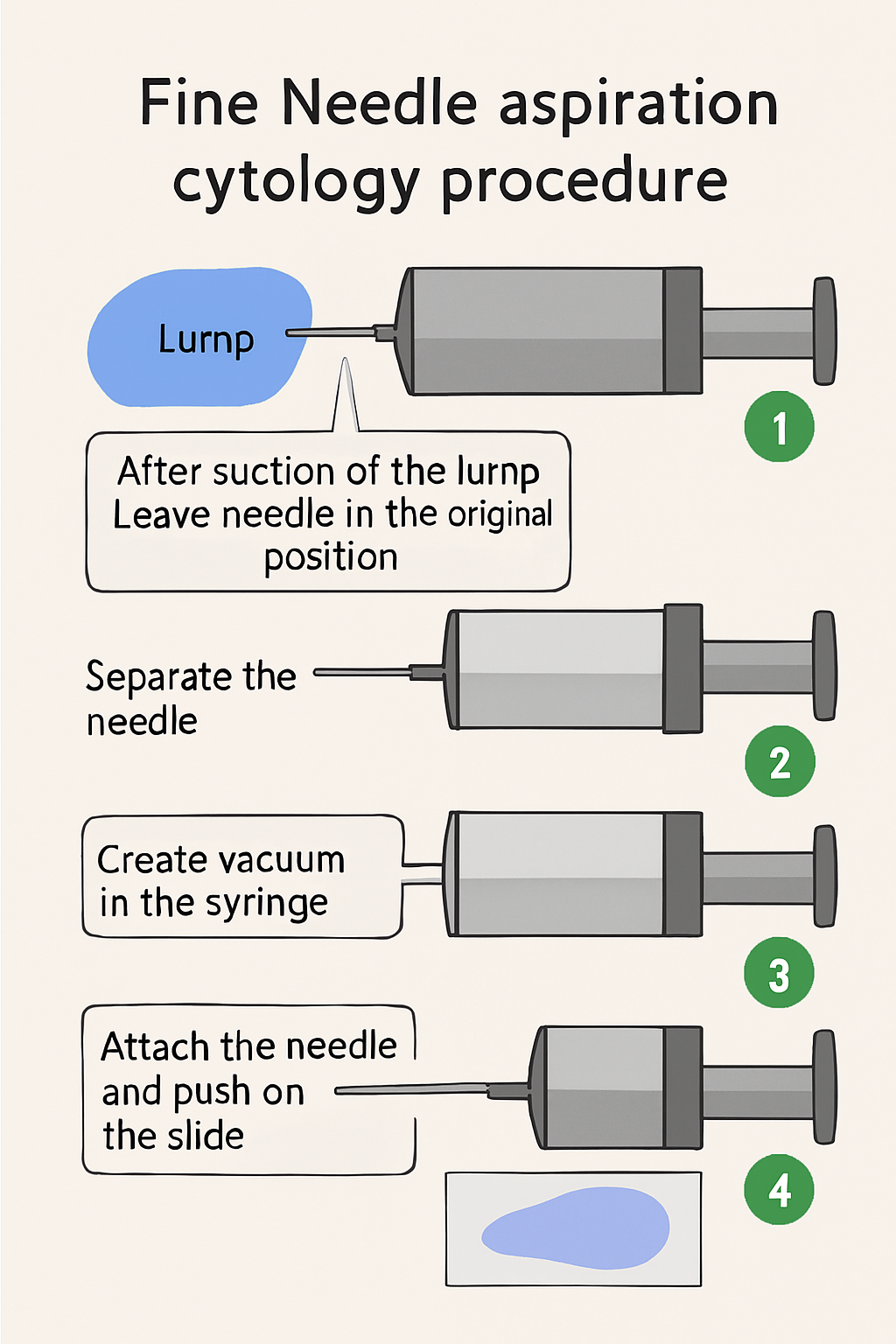
Fine needle aspiration Cytology (FNAC) with syringe procedure
Structured reporting systems have significantly enhanced the diagnostic utility of FNAC by promoting consistency, clarity, and clinical relevance. These systems utilise standardised terminology and category-based risk stratification to align cytological findings with clinical and radiological data, facilitating more informed clinical decision-making. Established frameworks such as the Bethesda System for Thyroid Cytopathology, the Milan System for Salivary Gland Cytopathology, and the Sydney System for Lymph Node Cytopathology provide well-defined diagnostic categories, associated malignancy risks, and evidence-based management recommendations. This standardisation reduces ambiguity, enhances interobserver agreement, and promotes effective communication between pathologists and treating physicians.
The integration of molecular cytopathology into FNAC practice is a significant advancement. With appropriate triage and sample preservation, cytology material can be used for molecular testing, enabling detection of actionable mutations, gene rearrangements, and expression profiles. This aligns with the principles of precision medicine, especially in thyroid cancers (e.g., BRAF, RAS, RET/PTC testing), salivary gland tumours (e.g., MYB-NFIB in adenoid cystic carcinoma), and lymphomas (e.g., clonality assessment via PCR).
In conclusion, FNAC remains an indispensable technique in pathology, offering a bridge between clinical suspicion and definitive diagnosis. When performed meticulously and reported using standardised systems, FNAC not only provides timely information but also reduces the need for more invasive procedures. As cytology continues to evolve with the integration of molecular diagnostics, FNAC will remain central to early, accurate, and personalised patient care.

Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in