Impaired striatal Glutamate/GABA regulation in violent offenders with antisocial personality disorder and psychopathy
Published in Social Sciences, Neuroscience, and General & Internal Medicine
Violent crime has enormous implications for society at a human and economic level. We know that the majority of this violence is committed by a small group of men who meet diagnostic criteria for antisocial personality disorder (ASPD). People with ASPD also do very poorly in most life outcomes, including employment, success with families, and physical health. Within this group, about one third also meet criteria for psychopathy. These individuals offend earlier, more often, and more severely throughout their lifetimes, and have even worse personal outcomes. There is a scarcity of treatment options for these people and a lack of good evidence to support those that we have. We know environmental factors influence the trajectory of the lives of those with ASPD, however, biology also plays a role – for example, genetic studies in large populations suggest a substantial contribution to offending behaviour. Hence, to develop effective treatments, we must develop a better understanding of the biological mechanisms underlying the condition.
What we already knew and what was missing
Studies in the last 20 years or so have begun to develop a model of brain irregularities in those with ASPD. Structural MRI studies have pointed to reduced volumes as well as wider variation in the cortex of those with ASPD compared to healthy subjects, while studies using functional MRI (fMRI) have shown that those with ASPD have abnormal patterns of brain activity when performing tasks that test responses to others’ emotions, and aspects of decision-making. While those with ASPD with psychopathy appear to have particular deficits in responding to emotions, those with ASPD with and without psychopathy appear to share decision-making deficits, at least to some degree. Work from neuroscience studies in animals and humans has shown that the neurotransmitter dopamine plays a crucial role in decision-making. Its activity is closely related to that of neurotransmitters glutamate and GABA, which together regulate the excitation and inhibition of neurons in the brain. Levels of dopamine cannot be measured directly in the brain, however the ongoing development of Magnetic Resonance Spectroscopy (MRS) technology has allowed for increasingly precise estimates of glutamate and GABA levels. However, very few studies have looked at glutamate or GABA levels in the brain in ASPD, and until now, none had examined their interplay in balancing brain excitation and inhibition in the form of a glutamate : GABA ratio. Importantly, no study had focused on a crucial decision-making region – the striatum.
What we did and what we discovered:
As part of a larger study also examining other aspects of brain function, we recruited three groups of men: two groups of violent offenders – one group with psychopathy and on group without psychopathy – and one group of healthy-non-offenders. We did not include individuals with major mental illness like schizophrenia or bipolar disorder, or those with serious neurological conditions. We monitored for drug use by participants and adapted our analysis to account for this. Every participant completed an MRS sequence as part of their MRI protocol. Our sequence examined glutamate and GABA levels in the striatum, allowing for a measurement of glutamate : GABA ratio in each participant. We carefully examined the quality of each participant’s set of data and excluded a small number who did not meet our quality control standard. In total, we included 30 violent offenders with ASPD (14 with psychopathy, 16 without psychopathy) and 21 healthy non-offenders.
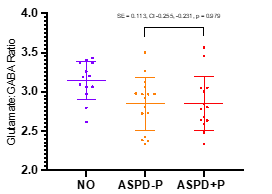
As a group, the violent offenders with ASPD had a significant reduction in striatal glutamate : GABA ratio compared to healthy non-offenders (‘NO’). Figure A shows the datapoints for this and the details of the statistical test showing a significant difference between these groups. There were no significant differences, however, between the offenders with ASPD with psychopathy and those without psychopathy, as shown in Figure B.
Figure A
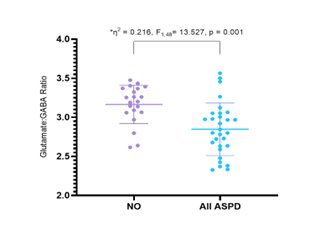
Figure B
What we concluded and what needs to be done next:
We have shown, for the first time, abnormal regulation of glutamate/GABA in the striatum in violent offenders with ASPD, with and without psychopathy. This has some especially important implications. First, it gives us a better understanding of how specific brain functions like decision-making may be impaired by neurochemical dysfunction, and provides a potential target for treatments that might correct this abnormality. This aspect, however, will require us to show a clear link between glutamate/GABA abnormalities and behavior, such as decision-making. This was not possible in this wider study due to time constraints, but will be an important component of future studies. Second, our findings give us a model to test in finer detail in animal studies. By testing the effect of drugs, including those in development for humans, on glutamate/GABA, these studies could in turn help guide future drug studies in humans. This is known as ‘back translation’ and is increasingly seen as a crucial component of translational impact. Finally, we discuss in our paper how, by linking glutamate/GABA to measures from other less invasive tests such as electroencephalography (EEG), we could develop simpler and less expensive ways of selecting out which subjects may be most suited to future treatment trials.
Overall, we believe this study is an important step in linking previous neuroimaging research in ASPD and psychopathy to a mechanistic understanding of the condition at a molecular level.
Follow the Topic
-
Molecular Psychiatry

This journal publishes work aimed at elucidating biological mechanisms underlying psychiatric disorders and their treatment, with emphasis on studies at the interface of pre-clinical and clinical research.
Your space to connect: The Psychedelics Hub
A new Communities’ space to connect, collaborate, and explore research on Psychotherapy, Clinical Psychology, and Neuroscience!
Continue reading announcement


Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in