Interconnected Epidemics: The Impact of My Research on Obesity, Metabolic Syndrome, Diabetes, and cardiovascular diseases
Published in Biomedical Research and Public Health
The publication of my perspective article, Interconnected Epidemics: Obesity, Metabolic Syndrome, Diabetes, and Cardiovascular Diseases: Insights from Research and Prevention Strategies, in the Discover Public Health journal is a significant milestone in my scientific journey. An article, a culmination of years of dedicated research, sheds light on the intricate web of non-communicable diseases (NCDs) and their overlapping risk factors, providing critical insights into prevention and intervention strategies. Here, I share the story behind this work, the challenges faced, the successes achieved, and its broader implications for future research and public health policies.
The Genesis of the Study
My research career has been shaped by an enduring commitment to understanding obesity and its related metabolic disorders study at King George’s Medical University, Lucknow, UP, India. The increasing global prevalence of obesity and metabolic syndrome is alarming, with these conditions acting as precursors to diabetes and cardiovascular diseases (CVDs). While working across clinical, preclinical, and public health settings, I observed a critical gap: despite extensive research on individual diseases, there was a lack of comprehensive studies integrating their interconnected nature.
This realization sparked the idea for my study-to bridge the gap between metabolic disorders and cardiovascular conditions by evaluating their shared pathophysiological mechanisms, genetic predispositions, and lifestyle-related risk factors. I envisioned a perspective that would not only analyse the published and existing data but also propose holistic prevention strategies aimed at mitigating the burden of NCDs globally.
Overcoming Challenges in Research
Every impactful study comes with its share of challenges, and mine was no exception. The interdisciplinary nature of this research required synthesizing findings from various scientific domains, including endocrinology, cardiology, genetics, and public health. Integrating these perspectives while maintaining scientific rigor was a formidable task.
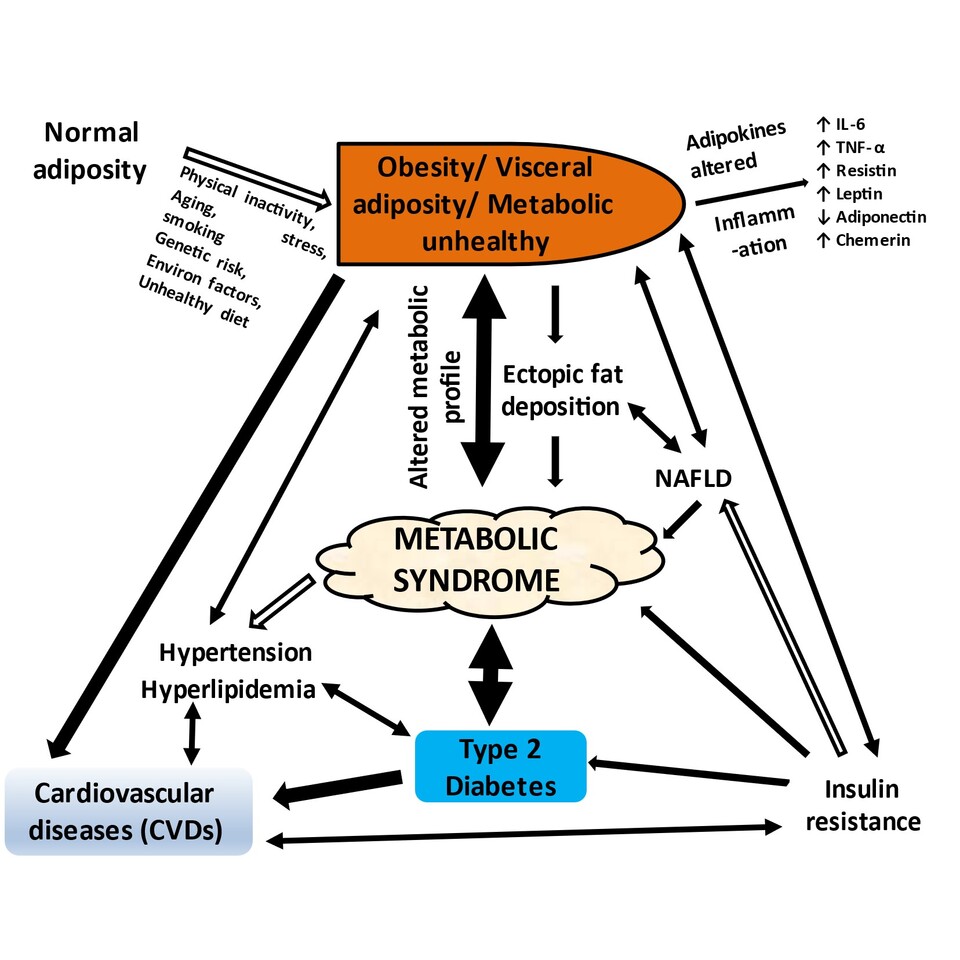
Another challenge was the complexity of analysing multifactorial interactions. The interplay between adipokines, insulin resistance, chronic inflammation, and genetic predisposition required a robust statistical approach. Collaborating with experts from diverse fields helped refine our analytical framework, ensuring that our conclusions were both scientifically sound and practically relevant.
Access to diverse population datasets was also a hurdle. Given the variations in genetic and environmental factors influencing metabolic disorders, it was crucial to use that data from different ethnic backgrounds. I worked with international research collaborators to include multiethnic cohorts, strengthening the study's applicability to global health challenges.
Key Findings and Contributions
Our research underscores the bidirectional relationship between metabolic syndrome and cardiovascular diseases, emphasizing that interventions targeting one condition must consider the broader metabolic landscape. Some key findings include:
- Adipokine Dysregulation and Cardiovascular Risk: We highlighted the role of adipokines such as adiponectin and leptin in modulating insulin sensitivity, inflammation, and vascular health. Dysregulation of these biomarkers serves as a critical link between obesity and CVDs.
- Genetic Predisposition and Lifestyle Factors: While genetic variations significantly influence metabolic syndrome risk, our study found that lifestyle modifications-such as diet, physical activity, and stress management-can mitigate genetic susceptibility, reinforcing the importance of preventive healthcare.
- Public Health Strategies for Disease Prevention: We proposed an integrated approach that combines early screening, community-based interventions, and policy-level changes to curb the rising tide of NCDs. A multi-sectoral strategy involving healthcare professionals, policymakers, and local communities is essential for impactful prevention.
Personal Anecdotes and Untold Stories
Scientific research is not just about numbers and analyses; it is also about the human stories that fuel our passion for discovery. I vividly recall a visit to a healthcare center, where I met patients struggling with multiple metabolic conditions due to limited access to healthcare. Their resilience and willingness to adapt to healthier lifestyles reaffirmed the importance of public health interventions.
Another defining moment was a conversation with a young researcher during an international conference, webinars, postdoctoral studies and various Institutional visits. They shared how the earlier publications on adipokine biomarkers had inspired them to pursue research in metabolic diseases. Such encounters remind me that our work extends beyond laboratories-it shapes the next generation of scientists and influences real-world health outcomes.
Implications for Future Research
While this study provides critical insights, it also opens doors for future research avenues. Advancements in precision medicine, gut microbiome studies, and digital health interventions hold immense promise for tailoring prevention strategies to individual risk profiles. Future studies should explore how emerging technologies, such as artificial intelligence and wearable health devices, can optimize early disease detection and intervention.
Additionally, given the increasing prevalence of metabolic disorders in younger populations, longitudinal studies tracking metabolic health from childhood to adulthood are imperative. Understanding early-life determinants of metabolic dysfunction will help design targeted preventive strategies.
A Call to Action for Public Health
The findings from my research (https://scholar.google.co.in/citations?user=xxFWuZUAAAAJ&hl=en) and https://www.researchgate.net/profile/Abhishek-Gupta-66 reaffirm the urgency of tackling obesity, metabolic syndrome, diabetes, and cardiovascular diseases as interconnected epidemics. Governments, healthcare institutions, and researchers must collaborate to implement sustainable policies that promote healthier lifestyles, enhance access to quality healthcare, and encourage early screening programs.
Moreover, the general public plays a crucial role in combating NCDs. Simple lifestyle modifications, such as adopting a balanced diet, engaging in regular physical activity, and managing stress, can collectively contribute to reducing disease burden. As researcher, it is our responsibility to do not only advance research but also translate our findings into actionable health strategies for communities worldwide.
Conclusion
My research journey has been one of perseverance, interdisciplinary collaboration, and a deep-seated commitment to public health. The acceptance of my study in Discover Public Health is not just a professional achievement but a testament to the collective efforts of researchers worldwide striving to combat the global NCD crisis.
As I look ahead, I am excited to explore new frontiers in metabolic disease research, mentor aspiring scientists, and contribute to shaping evidence-based public health policies. The battle against obesity and related metabolic disorders is far from over, but with continued research, innovation, and public engagement, we can make meaningful strides toward a healthier world.
Follow the Topic
-
Discover Public Health

This is an open access journal publishing research from all fields relevant to public health.
Related Collections
With Collections, you can get published faster and increase your visibility.
Public Health Strategies for the Management and Prevention of Tobacco Use and Emerging Tobacco Products
Tobacco use is considered as one of the hidden epidemics of the 21st century. Despite many efforts at policy level, tobacco use still remain one of the key factors for high morbidity and mortality worldwide. Globally around eight million people die due to tobacco consumption while daily people are diagnosed with lung cancer, COPD, cardiovascular diseases etc., with main factor being the tobacco consumption. Tobacco prevalence range between and within regions and countries as well as between male and female gender. Tobacco uses usually starts at adolescent and continue in the later life. At global level several initiatives have been undertaken with the WHO-FCTC being one of the most important. Additionally, at national levels countries have undertaken several initiatives but with not very successful results. On the other hand, tobacco industry is putting priority in the new products such as electronic cigarettes, heated tobacco etc. These products are not considered in many regions and countries as the normal tobacco products with their taxation, availability and use being different. To some extent, healthcare systems are not performing well in the management of the tobacco use which is considered a chronic condition. Availability of new medicaments and approaches and techniques is still a problem in many settings worldwide. Combination of tobacco use and other substances is also a critical issue.
This Collection aims to discuss key strategies for management of tobacco use and the new products at local, national, regional and global level as well as to propose key measures for healthcare personnel and policymakers in order to manage key challenges. Authors from different settings and different backgrounds are invited to submit their works to this Collection. Reviews and systematic analyses and meta- analyses, original articles, policy papers and case-studies are more than welcome to be submitted.
Research areas may include but are not limited to the following:
- Tobacco consumptions
- New tobacco products
- Prevention and management of tobacco use
- Substance use
- Technology and public health
- Prevention and health promotion
Keywords: tobacco, heated tobacco, public health, health policy, prevention and health promotion
This Collection supports and amplifies research related to SDG 3.
Publishing Model: Open Access
Deadline: Apr 30, 2026
Antimicrobial Resistance: The New Challenge to Global Health in a Post-Pandemic World
Antimicrobial resistance (AMR) is a seriously ongoing threat to global health, occurring when bacteria, fungi, viruses, and parasites evolve to resist the drugs designed to kill or block them. The COVID-19 pandemic has both directly and indirectly exacerbated the problem of AMR, as the overuse of antibiotics has accelerated the development of resistance in many pathogens. COVID-19 may have subsided, but AMR continues to pose a significant risk to the effectiveness of global healthcare systems, threatening to reverse decades of progress in combating infectious diseases. The interplay between population health and AMR has become increasingly critical as healthcare practices have shifted in response to the pandemic. Understanding this relationship is essential for developing effective strategies to mitigate the impact of AMR on population health in a post-COVID context.
The motivation for launching this Collection arises from the urgent need to address the rising tide of AMR as healthcare systems grapple with the long-term effects of the pandemic. Increased antibiotic use during COVID-19 treatment, changes in healthcare access, and disruptions in public health interventions have all contributed to an environment where AMR can thrive. Moreover, the pandemic has highlighted the importance of a multidisciplinary approach to tackling AMR, involving epidemiology, policymaking, and community health initiatives. This Collection aims to provide a platform for researchers and practitioners to share insights and findings that can inform future strategies to combat AMR while considering the broader implications for population health.
This Collection aims to highlight the multifaceted nature of AMR in a post-pandemic environment. We solicit articles that investigate the particular issues provided by the pandemic in terms of AMR development and containment, examine the impact of AMR on many sectors of healthcare, and propose novel strategies to minimize resistance propagation. Submissions may include original research, policy assessments, program evaluations, and comments on the following major areas:
• Epidemiology and trends of AMR post-pandemic
• Impact of COVID-19 on antibiotic usage
• Surveillance strategies for AMR
• AMR and stewardship
• Prevention and control measures to limit AMR spread
• Policies and programs to promote antibiotic stewardship
• Economic and social implications of AMR
• Global collaboration and initiatives to tackle AMR
By addressing these critical issues, this Collection aims to provide a comprehensive understanding of the emerging challenges in antimicrobial resistance in a post-pandemic world and to promote effective strategies to preserve the power of our current antimicrobials.
Keywords: antimicrobial resistance; COVID-19; antibiotics; global health; infectious diseases; public health; policy; prevention
This Collection supports and amplifies research related to SDG 3.
Publishing Model: Open Access
Deadline: Jun 30, 2026



Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in