Migrants Face Inequality in Cancer Diagnosis
Published in Social Sciences, Cancer, and Sustainability
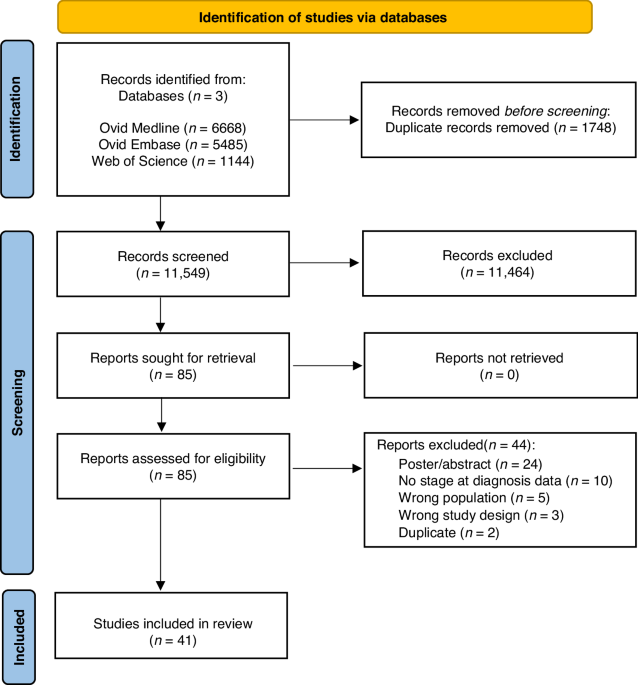
Working as doctors in the diverse communities of East London, we often see that migrants face significant challenges accessing healthcare. We see the real impact it has on their lives and premature deaths. Our newly published research shines a spotlight on this inequality. We demonstrated that among those diagnosed with cancer across OECD countries, migrants are 16% less likely to be diagnosed at an early stage compared with non-migrants (1). This delay risks a lower chance of survival, as early-stage cancers are usually more treatable than those diagnosed at a later stage.
Why Do Migrants Experience Inequality in Cancer Diagnosis?
We hypothesise that barriers to healthcare for migrants explains this inequality in cancer diagnosis. Barriers in access to and navigation of healthcare may result in delays in cancer diagnosis. Delays in diagnosis for migrants could explain the observed disparity in cancer stage at diagnosis.
The barriers that migrants face in accessing healthcare are well-described in the literature. They occur across multiple levels, with patient, clinician and healthcare system factors. We see (or, more worryingly, don’t see) these with our patients. The mother who delays seeing her doctor about a breast lump for fear of healthcare costs; the asylum seeker afraid that seeking healthcare will have an impact on their immigration status; the grandmother with limited English who doesn’t know the signs of cancer and didn’t understand the doctor’s advice to have further tests.
The Need for Further Research on Cancer Type and Migrant Experience
Our study demonstrated variation in inequality in cancer diagnosis according to cancer type and migrant background. Further research is needed to unpack these nuances.
Migrants are less likely to have early-stage diagnosis across different cancer types. Yet, variations were observed among different cancers. One of the most significant inequalities observed was in breast cancer. This is consistent with the study from Herbach and colleagues, which found that migrants were significantly less likely to be diagnosed with localised stage breast cancer (2). However, the association was weaker in other cancers like lung cancer. This variation may be partly due to limited studies for certain cancer types. But different cancer-, patient-, clinician- and health system factors can influence the diagnostic pathway for each cancer. Further research across cancer types is needed to understand what drives this variation. This would provide insights into how to address late diagnosis for specific cancers.
It is important also to consider that migrants are a diverse group. There is variation among migrants, within and between regions and across the migration journey. Some may be fleeing conflict, while others seek employment opportunities. Subgroup analysis in our study identified variation by region of origin of the migrant. Further research is needed to understand the differences across migrant groups. As well as by region of origin, future analysis of migrants could be stratified according to other factors. These could include reasons for migration, migration status, and duration of residence. Improved understanding will enable more personalised and effective interventions for specific migrant groups.
A Critical Policy Gap in Addressing Migrant Health Inequities
Across healthcare systems, improving both early cancer detection and health inequalities are priorities. In the UK, the NHS Long Term Plan prioritised early cancer detection, aiming for 75% of cancers to be diagnosed at an early stage by 2028. The NHS Core20PLUS5 approach to addressing health inequalities has a specific focus on early cancer diagnosis, featuring vulnerable migrants as an inclusion health group. Yet, current projections suggest that the target of 75% of cancer diagnoses made at stages 1 and 2 will not be met, whilst rates of early diagnosis remain lowest in ethnic minority and socioeconomically deprived groups.
Strategies to improve early cancer detection must consider migrant communities. They should include the co-development of evidence-based interventions targeted to reduce inequalities. These interventions should occur along the continuum of the cancer care pathway. They should also address the multiple patient-, provider- and system-level barriers to care. Example interventions include community-based health education tailored to migrant populations, training healthcare providers in cultural competency, improving provision of interpretation services and simplifying access to screening and follow-up appointments. Such targeted approaches could reduce the cancer inequities for migrant communities.
A Broader Need to Improve Migrant Health
Inequalities in cancer diagnosis are only one part of wider healthcare issues facing migrants. As highlighted in the accompanying editorial by Dee, there is a need to consider the experience of migrants through the lens of intersectionality (3). For many migrants, the obstacles to care begin long before they see a doctor. Limited access to stable housing, employment, and education compounds these barriers. This leaves them more vulnerable to delayed or missed diagnoses for various health conditions, not only cancer. Approaches to improve cancer diagnosis for migrants should learn from and contribute to wider efforts to improve migrant health.
Moving Forward: Collaborative Research, Policy Change, and Inclusive Care
As we encounter migrant patients in our East London communities, we hope that our research will help to address healthcare inequalities for them. Improving care for our communities requires targeted efforts for collaborative research, co-designed interventions, and broader reform.
- Harvey-Sullivan A, Ali S, Dhesi P, Hart J, Painter H, Walter FM, et al. Comparing cancer stage at diagnosis between migrants and non-migrants: a meta-analysis. British Journal of Cancer. 2024. https://doi.org/10.1038/s41416-024-02896-0
- Herbach E, Weeks K, O'Rorke M, Novak N, Schweizer M. Disparities in breast cancer stage at diagnosis between immigrant and native-born women: a meta-analysis. Annals of Epidemiology. 2019;40:39. https://doi.org/10.1016/j.annepidem.2020.09.005
- Dee EC. Cancer care for migrant people. British Journal of Cancer. 2024. https://doi.org/10.1038/s41416-024-02911-4
Follow the Topic
-
British Journal of Cancer

This journal is devoted to publishing cutting edge discovery, translational and clinical cancer research across the broad spectrum of oncology.




Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in