TB Care: Reimagined
Published in Microbiology

In his book To Repair The World, Paul Farmer warned us about the biggest challenge in global health - failures of imagination.
The most compelling example of this failure is how we manage tuberculosis. Even today, if you walked into an average TB clinic in an average high TB burden country, you will see century-old tools being used to diagnose and treat the leading infectious killer of humanity. The photo collage below is made up of real pictures that tell the story.

Chest radiology, tuberculin skin test, and sputum microscopy are tools that date back to the late 1800s, when pioneers like Wilhelm Rontgen and Robert Koch made landmark discoveries of their era. BCG, the vaccine we use today, dates back to the 1920s. We still use toxic drugs that make patients deaf, and we still rely on paper-based registers to keep track of patients and numbers. It is not surprising that TB continues to kill over 1.6 million people every year, and over 10 million people develop the disease annually. If this is not a collective failure of imagination, then I don't know what is!
In my spare time, I love to create PowerPoint slides on what my dream TB clinic would look like. The graphic below is my 'dream TB clinic.'
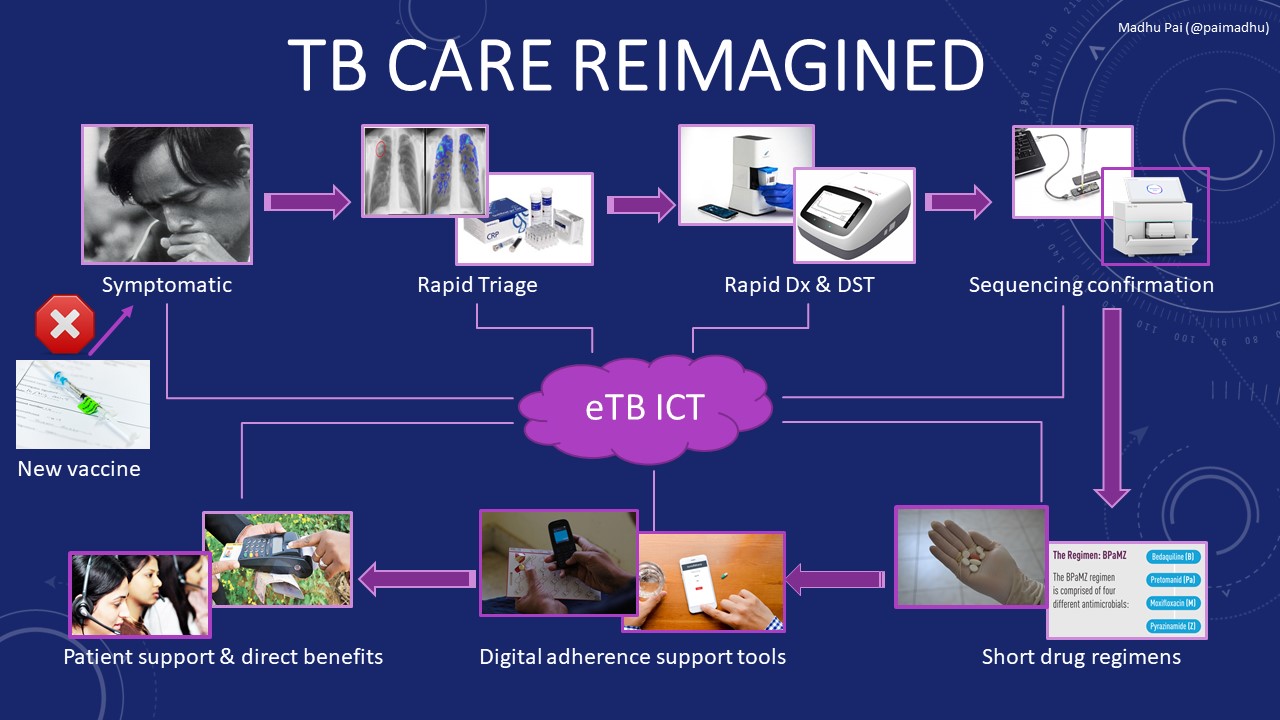
My dream clinic will include a much better TB vaccine to prevent new disease. A recent trial showed promise for a vaccine candidate called M72/AS01E (GlaxoSmithKline), shown in the graphic above.
For those who develop TB symptoms, we will offer a rapid, simple triage test. Efforts are underway to develop rapid, low-cost triage tests using biomarkers, while computer-aided software algorithms (which use AI) can now read digital x-ray images and help with rapid screening.
Those with positive triage test results will get a point-of-care molecular diagnosis, followed by confirmatory drug-resistance testing using sequencing. Such tools are already available (e.g. TrueNAT MTB by Molbio), or will soon be (e.g. GeneXpert Omni by Cepheid & Q-POC by QuantumDx) for point-of-care testing, while tremendous advances are being made in sequencing (e.g. MinION by Oxford Nanopore; iSeq by Illumina), which is becoming more feasible and affordable by the day.
People diagnosed with TB will receive a short four-month course of oral medicines. Such short regimens (e.g. a regimen called BPaMZ by TB Alliance) are in trials, with exciting early results. In fact, shorter treatments for latent TB infection (e.g. 4 months of rifampicin, and once-weekly isoniazid-rifapentine for 12 weeks) are already available.
Patients will have access to digital technologies that can help them stick to their treatment plan and allow them to receive direct benefits or money transfers. Digital adherence technologies (DATs)—which include feature phone–based and smartphone-based technologies (e.g. 99DOTS, SureAdhere Video DOT, Emocha) digital pillboxes (e.g. Wisepill) and ingestible sensors (e.g. Proteus) —may facilitate more patient-centric approaches for monitoring adherence. Call centers will be used to encourage patients to complete therapy and to link them to public services.
A modern TB service will be free of paper. And, thanks to cloud-based information and communication technologies (e.g. Everwell, Nikshay), TB program staff will be able to monitor the epidemic locally and nationally, as well as offering patients the personalized care and support they need.
Is this modern TB service an unrealistic dream? I don’t think so. As I have argued earlier, many such tools and solutions already exist, in some form or fashion (all the images I have used in the graphic above are real!). They have just failed to come to together to serve those who need them the most. And, for some tools such as a better vaccine and a shorter drug therapy, new investments are urgently needed.
Yes, developing new tools is going to cost money — an additional US$1.3 billion per year. But if the global health community can find a way to fight Ebola with modern tools and technologies, I see no reason for the TB field to be unambitious.
We can totally science the shit out of TB! The innovations I have described show that it is possible. My dream clinic could be up and running within the next couple of years. For that to happen, we need to counter our failures of imagination, and be more ambitious.
Photo credits: Many of the images were taken by me. Some were obtained from free online sources, or provided by agencies such as TB Alliance, Aeras, Everwell, SureAdhere, Cepheid, Molbio, Illumina and Oxford Nanopore.
Acknowledgements: This blog post is inspired by a presentation I was asked to deliver at the TB Innovation Summit in New York City, co-hosted by the Stop TB Partnership, Johnson & Johnson, World Economic Forum, UN Foundation, and the Global Fund to Fight AIDS, Tuberculosis and Malaria





Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in
Sir I am enlightened with your scientific views I wish to state that we have created a whats app group and publishing a e-new letter with title INFECTION CONTROL TRENDS I wish you to join our group on whats app +919961785124 and be our adviser and contribute a guest editorial to our upcoming e-newsletter on current thinking on Infectious diseases it will help many upcoming professionals in India and many other countries this e-newsletter is circulated to many regions in the world your help is highly appreciated
Dr.T.V.Rao MD ( Alumni Andhra Medical College Visakhapatnam India
Freelance clinical Microbiologist
Madhu,
I would remiss if I did not also highlight the digitization of diagnostic tests themselves (e.g. GxAlert) as part of that optimal lab vision. Simply by digitizing existing diagnostics, countries have saved millions in supply chain, improved case notifications, reduced diagnostic errors, assisted in getting patients enrolled onto treatment, and many other benefits.
More importantly, in addition to the individual digital tools you mention -- and most of them have generated fantastic results and evidence in their own right -- is the tremendous potential of connecting digital systems together, which results in incredible benefits. For example, by combining Riders4Health's digital specimen transport app/data with GxAlert's diagnostic results, one is able to track the whole clinic-to-lab-back-to-clinic TB testing process from start to finish. Such data was previously available only after conducting a 6-month study of paper logbooks riddled with errors, missing data, and partial entries. By connecting systems, you can see interim processes (e.g. delivery time, time in depot, lab turnaround time, results reporting time) and improve what you measure. Partial implementations of such connections led to quadrupling the test volumes in Ethiopia, cutting results delivery from 61 days down to <1 hour in Malawi, and saving $1m or more in supply chain optimization in Nigeria.
It's time for digital diagnostics to be connected with digital treatment, adherence, and patient benefits. It's time for digital triage (e.g. CAD4TB) to refer high-risk patients directly into digital diagnostics (GxAlert), and so on. And, it's time for funders and ministries to view these interventions as part of a connected whole and both execute as such. There is an opportunity for a visionary country to take the lead and implement against the strategy you lay out above. All of the interventions exist today and the benefits will compound immediately.
Best
Jeff Takle
Co-founder of GxAlert (SystemOne)
Thanks for these wonderful insights, Jeff. Fully agree!
Madhu