Asylum Seeker and Refugee Oral Health: the Barriers to Care and Why They Matter. A Systematic Review.
Published in Social Sciences, General & Internal Medicine, and Public Health

Why is this review important?
In the UK, we are used to hearing about asylum seekers and refugees (ASRs). We are bombarded with news of perilous channel crossings in dingeys, Bibby Stockholm and the Rwanda bill. Behind the headlines, we see real people, broken by war, trying to heal and make a new life. This systematic review sheds light on the healthcare inequalities faced by asylum seekers and refugees (ASRs) and suggests some ways we can make this right.
The opportunity to conduct this research presented itself when my supervisor, Dr Jo Morling, suggested it as my dissertation project. I began with very little knowledge of oral health (as I’m training to be a medic this has always been outside of my scope of knowledge); however, I was drawn to this research with a great hunger for justice in healthcare. Why do ASRs have poorer oral health? To answer this question, we conducted a systematic review of the relevant literature. We searched 5 electronic databases and after applying exclusion criteria we analysed 13 primary studies.
What did we find?
We found that ASRs suffer from poorer oral health and find it difficult to access care in their host countries. Specifically, we identified three barriers and two facilitators to oral healthcare for ASRs. More detailed findings of can be found in Figure 1, however, to summarise the main themes:
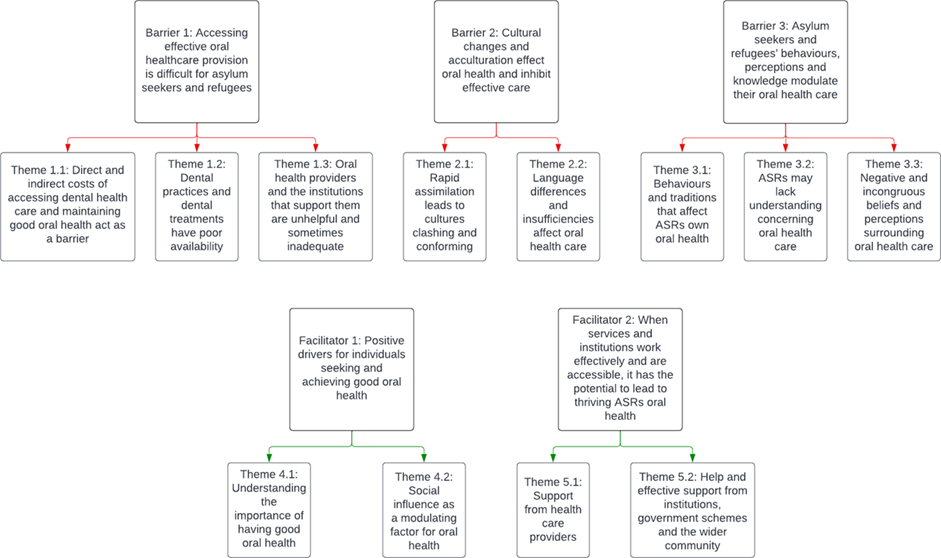
Figure 1: theme map of barriers and facilitators to oral healthcare for ASRs.
- Barrier 1: The cost of dentists, transport and toothpaste are often barriers to accessing care for ASRs. Dental practices have low availability and often cannot accommodate the unique care needs of refugees.
“The first time I went, they gave me a 2 months appointment and eventually I forgot I had that appointment.” (1)
- Barrier 2: The clash of cultures means that care is not delivered in the most effective way. This manifests as language differences and contradictory messages, leading to uncertainty and confusion.
“It is the language problem; I can’t tell a dentist what is really happening to me, and that is why I didn’t go to them [dentists]” (2)
- Barrier 3: Refugees’ own personal knowledge, perceptions, cultural beliefs and behaviours negatively impact when care is sought and how they engage with care.
“If we use the toothbrush frequently, with toothpaste after every meal, I believe that it may damage our tooth” (2)
However, we didn’t just identify barriers to care, many things were referenced as positive facilitators to good oral healthcare access and wider oral health quality:
- Facilitator 1: Social influence from peers and role models can encourage people to seek oral healthcare and understand the importance of having healthy teeth.
“Back in Pakistan or Afghanistan [brushing your teeth] was like not to be honest it was not like an everyday thing...now that I think about it it's kinda gross, but it wasn't to be honest but here when we came it's like uh everybody cleans their teeth twice a day.” (3)
- Facilitator 2: When support is provided by healthcare providers, government schemes and the wider community, - it can lead to thriving oral health.
“As my former dentist is so cooperative, I also take many of my fellow Eritreans, who don’t understand about their dental health, to her and get the treatment” (2)
“I think refugees like me will never be able to pay for dental treatment if not for the government insurance.” (4)
Many of these findings are supported by previous literature narratives (5, 6) - however, some themes identified are unique to this review. Namely the impact that acculturation, assimilation and social influence have on ASRs oral health.
Where do we go from here?
There is clearly a need for societal change to break down the identified barriers and improve ASR’s oral health and quality of life. We have suggested a few ways to do this. There is a need to educate communities and provide them with oral healthcare tools such as toothbrushes. Healthcare staff should be trained in cultural competency and made aware of care pathways, and translators should be widely available. Institutional changes, such as increased communication between policy makers and healthcare providers, financial support and local projects such as mobile clinics may alleviate some of these barriers to good care and facilitate better care standards. If made, research should then investigate how effective the changes have been. It is important oral health is improved, as this positively affects employment, happiness and other areas of health.
Given that new conflicts arise every year for ASRs, this research and any change to policy should be continually evaluated to ensure care remains effective.
Conclusion
ASRs suffer from poor oral health and from poor access to oral healthcare due to systemic and cultural barriers. With greater education, training and funding, these barriers could be alleviated.
I found this research challenging having never done a systematic review before; however, it was a steep learning curve, and I didn’t expect the process to be as fruitful as it has been. My supervisor and second author have helped me realise how research can change the lives of vulnerable groups in society. If our suggested changes are implemented it could help survivors of war integrate into society and begin the process of healing.
Thank you for reading and please share this blog and read the full article at https://doi.org/10.1038/s41415-024-7235-9. All claims in this blog can be supported by references in the full paper.
References
- Nurelhuda NM, Keboa MT, Lawrence HP et al. Advancing Our Understanding of Dental Care Pathways of Refugees and Asylum Seekers in Canada: A Qualitative Study. International Journal of Environmental Research and Public Health. 2021;18(16):8874. Advancing Our Understanding of Dental Care Pathways of Refugees and Asylum Seekers in Canada: A Qualitative Study - PMC (nih.gov)
- Kidane YS, Ziegler S, Keck V et al. Eritrean Refugees’ and Asylum-Seekers’ Attitude towards and Access to Oral Healthcare in Heidelberg, Germany: A Qualitative Study. International Journal of Environmental Research and Public Health. 2021 Nov 3;18(21):11559. Eritrean Refugees’ and Asylum-Seekers’ Attitude towards and Access to Oral Healthcare in Heidelberg, Germany: A Qualitative Study - PMC (nih.gov)
- Due C, Aldam I, Ziersch A. Understanding oral health help‐seeking among Middle Eastern refugees and asylum seekers in Australia: An exploratory study. Community Dentistry and Oral Epidemiology. 2020 Jun;48(3):188-94. Understanding oral health help‐seeking among Middle Eastern refugees and asylum seekers in Australia: An exploratory study - Due - 2020 - Community Dentistry and Oral Epidemiology - Wiley Online Library
- Keboa MT, Hovey R, Nicolau B et al. Oral healthcare experiences of humanitarian migrants in Montreal, Canada. Canadian Journal of Public Health. 2019 (b) Aug 15; 110:453-61. Oral healthcare experiences of humanitarian migrants in Montreal, Canada | Canadian Journal of Public Health (springer.com)
- Paisi M, Baines R, Burns L et al. Barriers and facilitators to dental care access among asylum seekers and refugees in highly developed countries: a systematic review. BMC Oral Health. 2020 Dec;20(1):1-0. Barriers and facilitators to dental care access among asylum seekers and refugees in highly developed countries: a systematic review - PMC (nih.gov)
- Bhusari S, Ilechukwu C, Elwishahy A, et al. Dental caries among refugees in Europe: a systematic literature review. International Journal of Environmental Research and Public Health. 2020 Dec;17(24):9510. Dental Caries among Refugees in Europe: A Systematic Literature Review - PMC (nih.gov)
Follow the Topic
-
British Dental Journal

This is an international, peer-reviewed journal for the dental community, published by Springer Nature on behalf of the British Dental Association.
Related Collections
With Collections, you can get published faster and increase your visibility.
Periodontology
Publishing Model: Hybrid
Deadline: Jun 30, 2026




Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in