Behind the Paper: How Higher BMI Increases Risks After Loop Ileostomy Surgery
Published in Biomedical Research, General & Internal Medicine, and Surgery

What Is a Diverting Loop Ileostomy?
A loop ileostomy is a surgically created opening in the abdomen where a loop of the small intestine (ileum) is brought out to the skin. Waste exits through this opening into a bag, diverting it from the lower part of the bowel. When parts of the lower bowel are cut out and stitched together in what is called an anastomosis, there is a small chance of a leak. Preventing stool from crossing where the anastomoses were made means that any leaks that develop will be less severe. Bowel resection and anastomosis are commonly performed for:
- Colorectal cancer surgery
- Inflammatory bowel disease (Crohn’s, ulcerative colitis)
- Diverticulitis
Once healing is complete, the stoma is reversed, and bowel function is restored.
Why Does BMI Matter?
Obesity (BMI ≥30) and overweight status (BMI 25–30) are known to increase surgical risks, including:
- Infections
- Poor wound healing
- Hernias
But until now, there hasn’t been a comprehensive look at how BMI specifically impacts DLI-related complications.
Key Findings: How BMI Affects Complications
After reviewing 5,141 patients, we found:
1. Stoma-Site Incisional Hernias Are Much More Common with Higher BMI
- All 7 studies reporting this complication found a strong link with BMI.
- Patients with BMI >25 had 4.7 times higher odds of developing a hernia.
Why? Excess weight puts more strain on the abdominal wall, making hernias more likely after stoma closure.
Meta-analysis result:
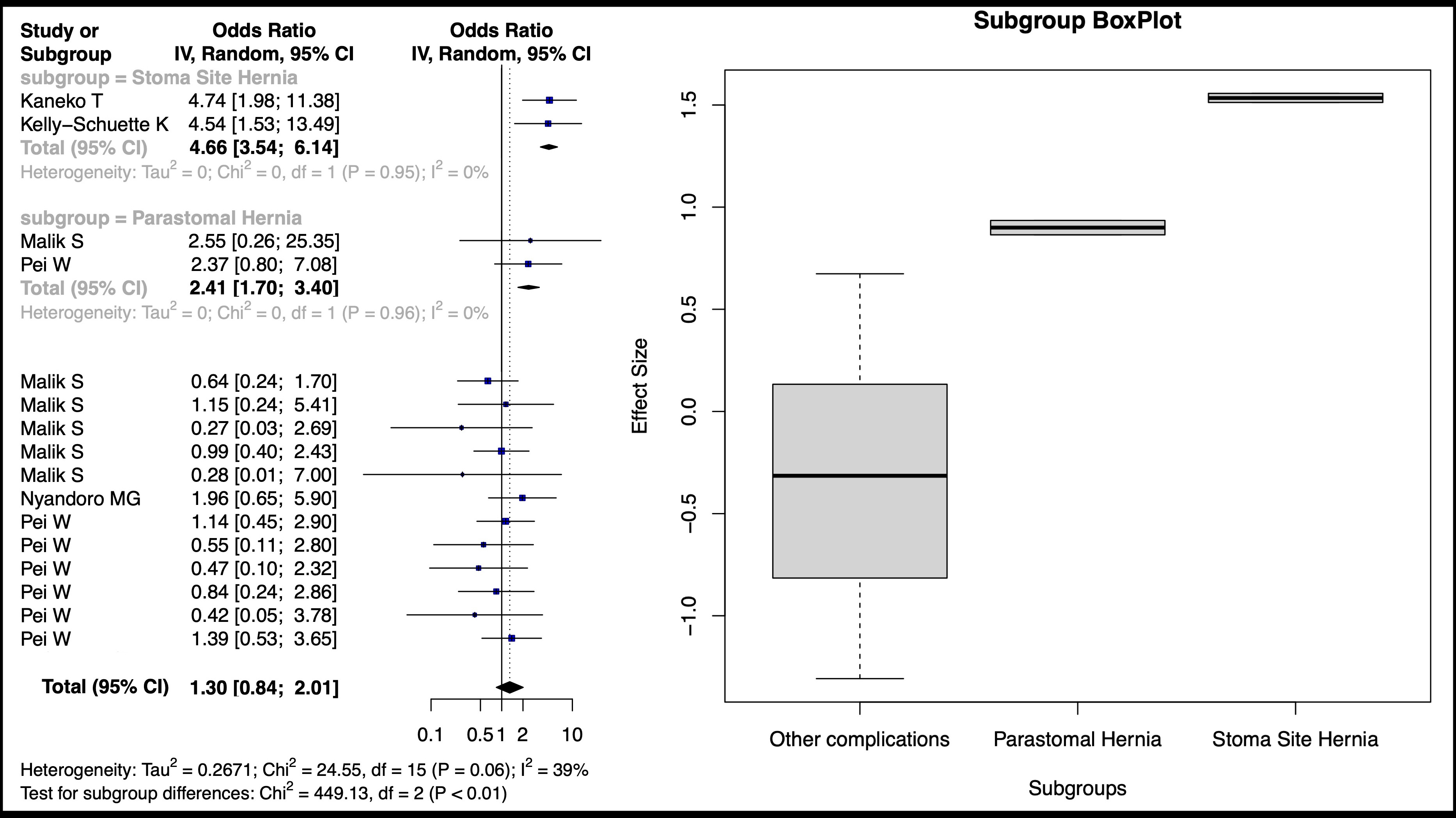
Forest plot of calculated log odds ratios for complications occurring over BMI 25 for included studies. Notes: The random-effects meta-analysis model (Inverse Variance method) was used. Abbreviations: Cl, Confidence Interval; df, degrees of freedom; IV, inverse variance; Std, Standard
2. Other Complications Linked to Higher BMI
- Peristomal skin irritation (40% of studies)
- Delayed stoma reversal
- Higher overall complication rates in BMI >30 patients
3. Complications That Didn’t Appear to be Affected by BMI
- High-output Ileostomies (excessive fluid loss)
- Stoma retraction
- Death rates
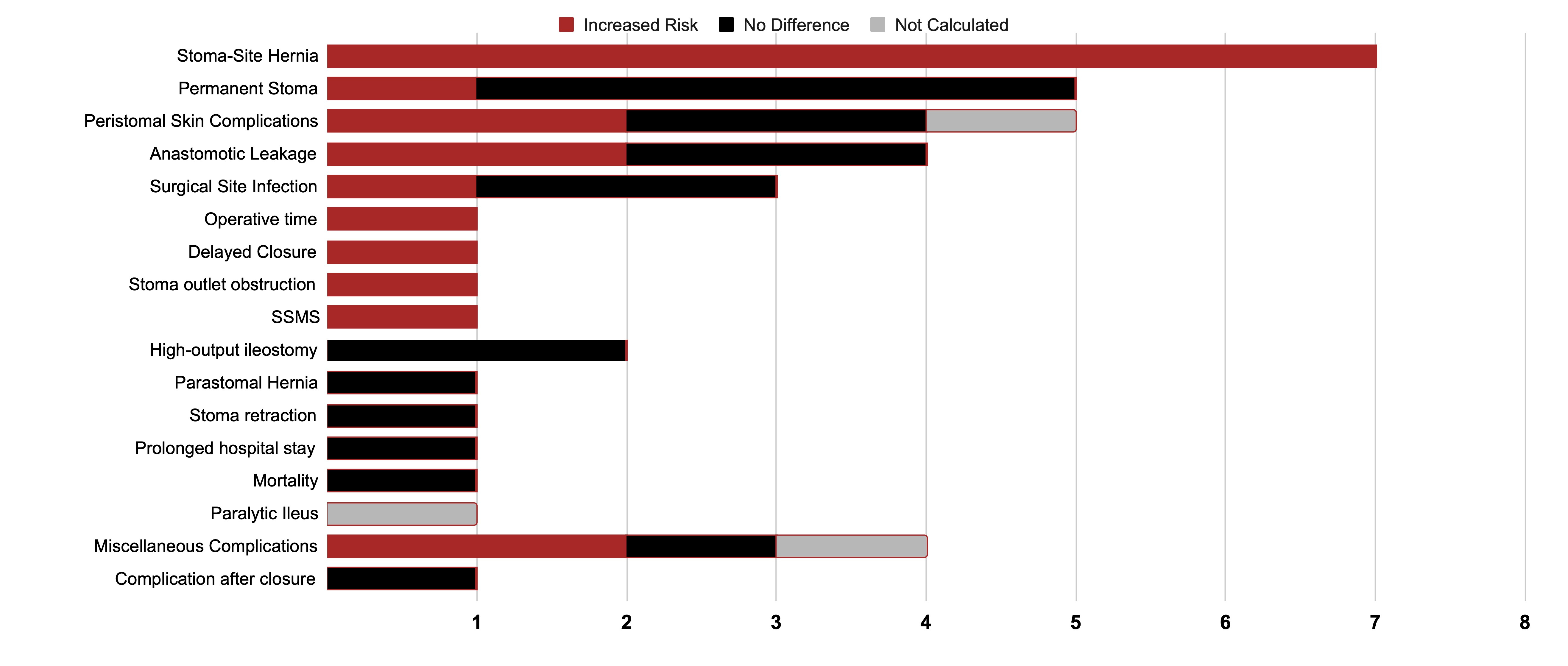
Complications affected by increased BMI
What Can Patients & Surgeons Do?
For Patients:
- Weight management before surgery may reduce risks.
- Monitor for hernias: bulging near the stoma site after reversal should be checked.
- Proper stoma care can prevent skin irritation.
For Surgeons:
- Consider preventative mesh placement at the stoma site for patients with BMI >25 to prevent hernias.
- Purse-string skin closure (instead of linear closure) may lower infection risks.
- Inform patients of elevated risks and consider delaying surgery to optimize weight if feasible.
Why This Study Matters
Our research provides evidence-based guidance for surgeons and patients:
- Higher BMI results in higher hernia risk, so mesh reinforcement should be considered.
- Weight loss before surgery could improve outcomes.
- More research is needed to decide which patients must delay surgery until their weight is optimized, and which patients may proceed with surgery given the higher risks.
Final Thoughts
If you’re preparing for a loop ileostomy, discussing BMI-related risks with your surgeon can help tailor your care plan. For the medical community, our findings highlight the need for targeted strategies to reduce complications in higher-BMI patients.
Read the full study here: https://doi.org/10.1007/s00464-025-11887-y
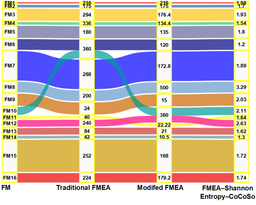
Visual Summary
Infographic: How BMI Affects Loop Ileostomy Outcomes

About the Authors
Kaiser Sadiq, MBBS, earned his medical degree from JIPMER, one of India's premier medical schools. He was a practicing general physician in India and is currently a research fellow in the Division of Colorectal Surgery at UC San Diego. He has authored several peer-reviewed articles and is an incoming General Surgery resident at The George Washington University. This study was conducted with colleagues from UC San Diego and Abington Jefferson Hospital.
---
Have questions or thoughts on this research? Leave a comment below!
Disclaimer: This article is for informational purposes only and not medical advice. Consult your doctor for personalized guidance.
Follow the Topic
-
Surgical Endoscopy

This journal is a focal point for the international surgical community to exchange information on practice, theory, and research, positioned at the interface between various medical and surgical disciplines.




Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in