Behind the Paper: Intersecting Impacts of Ageing, Migration, and Socioeconomic Disparities on Health Equity – A Post-Pandemic Policy Review
Published in Social Sciences, Anatomy & Physiology, and Law, Politics & International Studies
The Story Behind the Paper
The Spark From Observation to Question
During the pandemic, we witnessed older adults in nursing homes devastated by COVID-19, migrant labourers losing their jobs and social protections, and low-income communities suffering high infection rates and poor access to care. These patterns felt connected. For example, an ageing migrant worker living precariously, lacking protection, and exposed to the virus illustrates overlapping vulnerabilities that erode health resilience.
In Ghana and many low- and middle-income countries, age-related care gaps, internal and external migration, and informal work intersect. We asked what the evidence reveals when ageing, migration, and socioeconomic inequality are examined together. How did the pandemic deepen these links, and what policy gaps emerged?
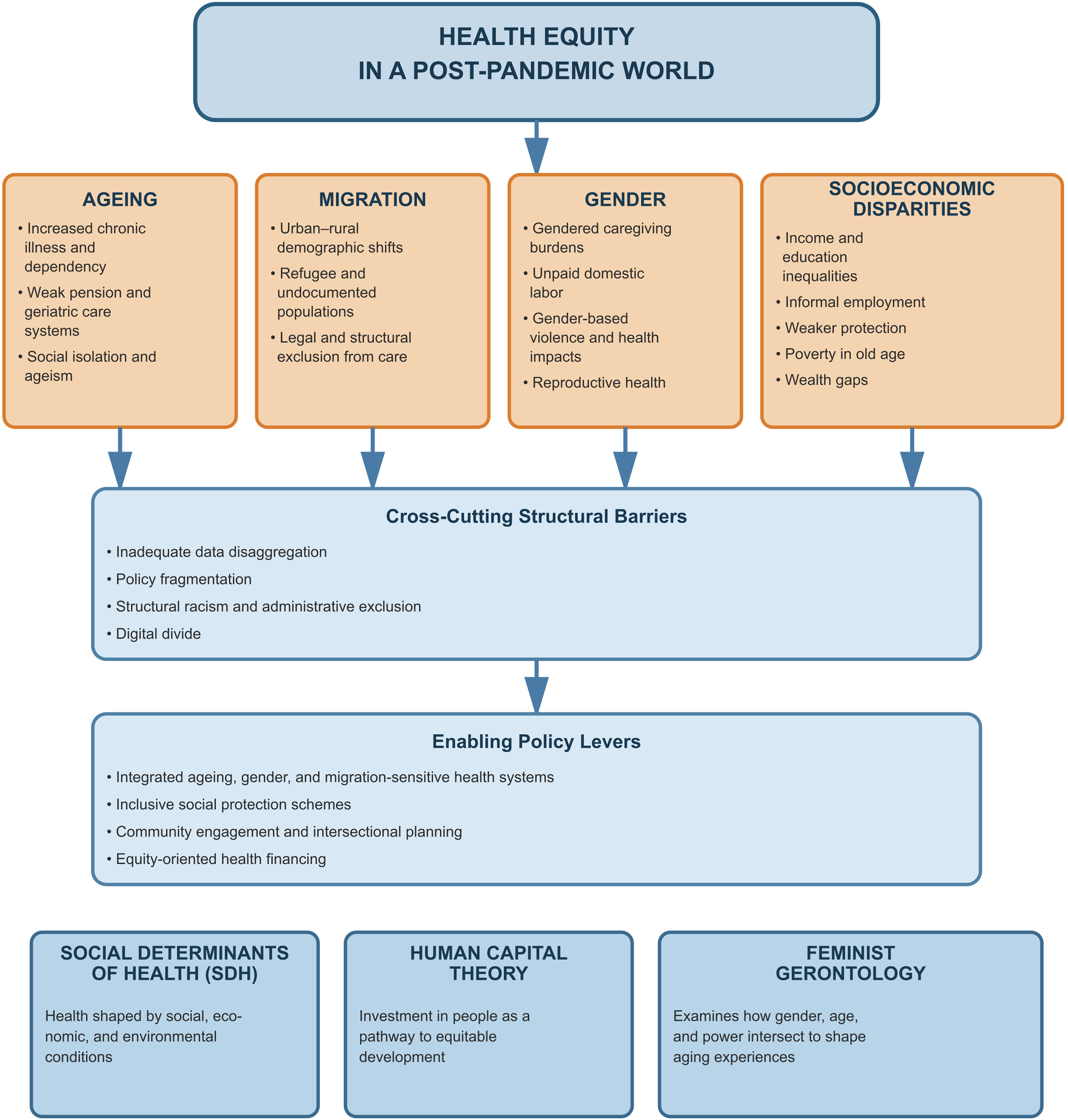
Conceptual Framing: Bringing Theory to Life
We grounded the study in three theoretical lenses
Social Determinants of Health (SDH) explains how living and working conditions, social protection, and public policy shape health outcomes.
Human Capital Theory, which considers how investment or disinvestment in health and skills influences lifetime resilience.
Feminist Gerontology, which captures ageing as a gendered life course process and highlights the burdens borne by older women and ageing migrants.
Our premise is that ageing, migration, and socioeconomic disadvantage are not additive. They intersect to multiply risk. The pandemic was a global stress test of this reality.
Methodology Systematic Review of the Policy Terrain
Following PRISMA 2020 guidelines, we preregistered our protocol on the Open Science Framework (OSF) and reviewed studies, reports, and grey literature from 2020 to 2024 that linked ageing, migration, and socioeconomic factors to health equity. In total, 49 sources met inclusion standards.
Key Findings: Four Intersecting Themes
-
Demographic inequality and uneven exposure. Older adults, migrants, and low-income groups faced the greatest risk with limited protection.
-
Exclusionary health systems and digital divides. Health systems often lacked ageing and migrant-sensitive services, and unequal digital access worsened inequities.
-
Socioeconomic precarity, job losses, informal work, and weak social protection eroded human capital.
-
Fragmented policy responses. Post-pandemic strategies rarely integrated ageing, migration, and poverty, creating blind spots in design.
Comparative analysis showed these gaps were most severe in the Global South, where social protection and health infrastructure remain weak.
The Ghana Africa Lens and Why It Matters
Although global in scope, the review is deeply relevant to Ghana and similar contexts. Ageing, migration, and economic disparities intersect sharply across rural-urban divides and informal economies. Older migrants and rural elders often lack pensions, insurance, or digital access. Integrating these realities bridges global evidence with local policy relevance.
Policy Implications Beyond Health Care
Health equity cannot be achieved through clinical reforms alone. We recommend
-
Age and migrant-inclusive health system design
-
Comprehensive social protection coverage for informal and cross-border workers
-
Bridging the digital divide in healthcare access
-
Institutionalising intersectional policy design across ministries and agencies
Why the Timing Matters
Published in November 2025, this paper arrives as the world rebuilds from COVID-19. Without embedding ageing and migration into recovery strategies, cycles of cumulative disadvantage will persist. Our review aims to inform that global reckoning.
Personal Motivation and Ethical Imperative
For us as Ghanaian scholars, this study transcends academia and represents an ethical duty. Older adults, migrants, and low-income persons remain invisible in many policies. We sought to make their experiences visible and call for governance that upholds dignity and inclusion across Africa and the Global South.
Conclusion
This paper bridges divides between ageing and migration studies, health policy and social protection, and research and justice. We hope to advance a conversation where no older migrant is left behind and no low-income community is forgotten in future crises.
Follow the Topic
-
International Journal for Equity in Health

This journal presents evidence relevant to the search for, and attainment of, equity in health across and within countries and publishes research which improves the understanding of issues that influence the distribution of health and healthcare within populations.
Related Collections
With Collections, you can get published faster and increase your visibility.
Racism and Health
The ongoing advancement of our understanding of how racism impacts health - both directly and structurally - is crucial for addressing the deep-rooted health inequities that persist globally. Structural racism shapes health outcomes among racialized populations, contributing to inequities in healthcare access and quality, and impacting social, political, or environmental determinants of health. Existing research also connects direct and visible manifestations of racism, such as major and everyday discrimination, to negative health outcomes. At the same time, racism does not operate in isolation. A growing body of research shows how it intersects with other systems of oppression—such as classism and patriarchy—and with broader social determinants of health, producing compounded and context-specific inequities. An intersectional lens is therefore essential to understand how overlapping structures of power and exclusion shape health and healthcare experiences. These insights are essential in conducting rigorous and thorough health research, guiding anti-racist health policy, and ultimately, ensuring equitable health for all.
Looking forward, research holds the potential to develop new methodologies and indices and unveil complexities in how racism manifests within healthcare systems and societal structures. By deepening our collective understanding, we can develop more effective interventions that target the root causes of health inequities.
We invite researchers to contribute to this special Collection on Racism and Health, focusing on advancing our understanding and addressing health inequities. Topics of interest include but are not limited to:
- Racism as a structural determinant of health
- Racism as a direct determinant of health
- Racialized health outcomes in different populations
- Intersectionality and inequities in health, healthcare access and quality
- Nexuses between social, political, and environmental determinants of health and systemic discrimination
- Anti-racist health policy frameworks and systems
- Impact of racism on mental health
- Health inequities in reproductive, maternal, and child health
- Obstetric and reproductive violence
- Community-based interventions for equitable health
- Decolonizing health research and global health epistemologies
We strongly encourage contributions from racialized scholars and authors with lived experience or expertise in addressing systemic discrimination in health research.
This Collection supports and amplifies research related to SDG 3, Good Health and Well-Being and SDG 10, Reduced Inequalities.
All submissions in this collection undergo the journal’s standard peer review process. Similarly, all manuscripts authored by a Guest Editor(s) will be handled by the Editor-in-Chief. As an open access publication, this journal levies an article processing fee (details here). We recognize that many key stakeholders may not have access to such resources and are committed to supporting participation in this issue wherever resources are a barrier. For more information about what support may be available, please visit OA funding and support, or email OAfundingpolicy@springernature.com or the Editor-in-Chief.
Publishing Model: Open Access
Deadline: Aug 14, 2026
Mental Health Inequities in Crisis: Insights from South-East Asia
The importance of advancing our collective understanding of mental health disparities during extraordinary crises, particularly in South-East Asia, cannot be overstated. As the region faces a multitude of challenges—ranging from natural disasters to public health emergencies—there is a pressing need to explore the variations in mental health impacts across different communities. Significant strides have been made in this area, including the identification of specific risk factors, the implementation of culturally sensitive interventions, and the recognition of mental health as a critical component of overall well-being. However, much work remains to be done. Future research has the potential to uncover new insights into the social determinants of mental health, enhance intervention strategies, and inform policies that promote equity. By deepening our understanding of these issues, we can better address the unique mental health challenges faced by vulnerable populations in the region.
We welcome all article types, including original research, reviews, meta-analyses, and perspectives.
We invite researchers to contribute to this special Collection. Topics of interest include but are not limited to:
-Socioeconomic & Geographic Disparities in Mental Health Access
-Community-Level Heterogeneity in Mental Health Outcomes
-Social Determinants of Mental Health in Crisis Contexts
-Culturally Adapted Mental Health Interventions
-Youth Mental Health in Crisis: Vulnerability and Resilience
-Gender and Mental Health: Differential Impacts and Responses
-Stigma, Barriers, and Facilitators to Mental Health Care
-Digital Mental Health Innovations in Low-Resource Settings
This Collection supports and amplifies research related to SDG 3, Good Health and Well-Being.
All submissions in this collection undergo the journal’s standard peer review process. Similarly, all manuscripts authored by a Guest Editor(s) will be handled by the Editor-in-Chief. As an open access publication, this journal levies an article processing fee (details here). We recognize that many key stakeholders may not have access to such resources and are committed to supporting participation in this issue wherever resources are a barrier. For more information about what support may be available, please visit OA funding and support, or email OAfundingpolicy@springernature.com or the Editor-in-Chief.
Publishing Model: Open Access
Deadline: Jul 30, 2026

Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in
Thank you, Yuanxin, for engaging with my post and for the work you do in building scholarly connections across the Springer Nature Research Communities. I truly appreciate the visibility this platform gives to early career researchers and the spirit of collaboration it fosters across disciplines.
Thank you for your contribution and I'm glad you like the Communities. Here is the Welcome course which can help you discover how to make the most of the Communities: https://communities.springernature.com/courses/1964