Behind the Paper: Revolutionizing Epiglottic Cyst Treatment with Videolaryngoscope-Assisted Coblation
Published in General & Internal Medicine and Surgery

Epiglottic cysts (ECs), although generally benign, can cause significant symptoms like globus sensation, dysphagia, and even airway obstruction in severe cases. Traditional surgical approaches for removing these cysts, such as direct laryngoscopy (DL), are effective but come with inherent risks, including mucosal injuries, dental damage, and even life-threatening complications in certain patients. The motivation to develop a safer and more effective approach led to our innovation: Videolaryngoscope-Assisted Coblation of Epiglottic Cysts (VACECs).
The Problem with Traditional Methods
Epiglottic cysts are often managed surgically when they become symptomatic or show potential to compromise the airway. Conventional techniques like DL are performed using a suspension laryngoscope. However, DL methods exert significant pressure on the oropharyngeal tissues and teeth. For patients with loose anterior teeth, dentures, or compromised oral structures, the risk of tooth loss and other complications becomes exceptionally high.

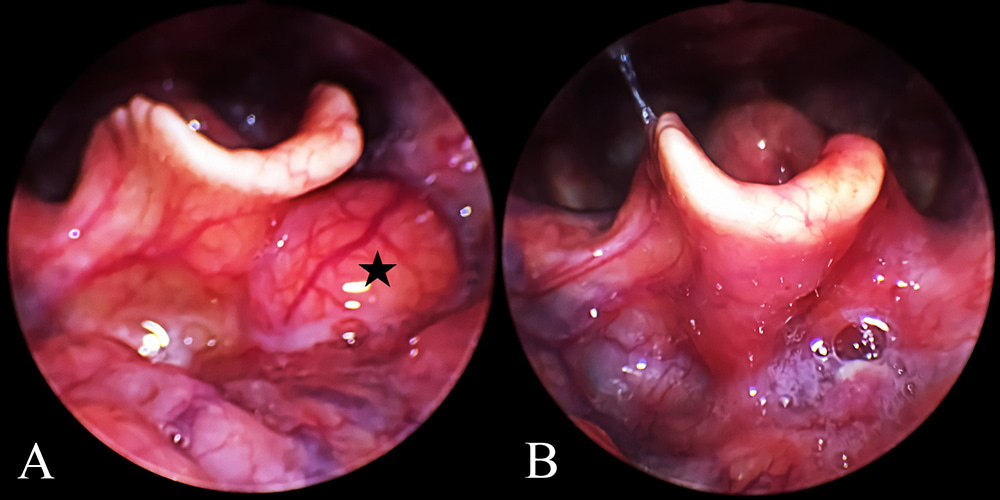
The image included here demonstrates the fragile dental structure we often encounter. A traditional DL-based procedure on such patients could easily result in tooth dislodgement and other adverse events, underscoring the need for a more refined surgical method. These observations inspired the development of our new approach, which is designed to minimize these risks while ensuring effective cyst removal.
Our Innovative Approach: VACECs
Videolaryngoscope-Assisted Coblation is a minimally invasive surgical technique that utilizes the videolaryngoscope, initially developed for intubation and airway management, in combination with coblation technology. This approach offers several advantages:
- Minimal Damage: The curved design of the videolaryngoscope reduces pressure on oral tissues and eliminates the risk of dental injuries. It does not require a direct line of sight, significantly lowering the mechanical strain on the patient’s head and neck.
- Curved Manipulation: Our method allows for precise, curved movements that are more anatomically suitable. The coblation device can be maneuvered smoothly to reach the cyst, avoiding damage to surrounding structures.
- Reduced Postoperative Reaction: Coblation technology ablates tissue at lower temperatures (40°C-70°C), minimizing thermal damage and promoting quicker recovery with fewer complications.



How We Conducted the Study
Between January 2015 and March 2019, we enrolled 28 patients at the Department of Otolaryngology, Wuxi Huishan District People’s Hospital. Our inclusion criteria ensured we had a diverse patient group, with ages ranging from 24 to 78 years, and various cyst sizes, from 0.8 to 1.5 cm. Each patient underwent a thorough preoperative assessment using electronic flexible laryngoscopy or a 70° rigid laryngeal endoscope to evaluate cyst location and size.
Under general anesthesia, the patient was positioned supine, and the videolaryngoscope was carefully inserted to expose the epiglottis and cyst. Using a coblation wand specifically bent to match the curvature of the videolaryngoscope blade, the surgeon performed precise cyst ablation. The real-time image on the display allowed us to control the operation with high accuracy, minimizing the risk of damaging adjacent tissues or dental structures.
The coblation wand’s integrated suction system effectively cleared cyst fluid and any minor bleeding, ensuring a clear surgical field. The entire procedure was completed in 10 to 20 minutes, demonstrating both efficiency and safety.
Results and Key Outcomes
Our outcomes were impressive: all 28 patients recovered without recurrence or significant complications. Postoperative follow-ups, conducted over more than half a year, confirmed the effectiveness of the VACEC procedure. None of the patients experienced tooth loss, even those with preexisting dental fragility. There were also no oropharyngeal injuries, and patients reported minimal postoperatively discomfort.
This success highlights how combining videolaryngoscopy with coblation can transform surgical practice in otolaryngology, making it safer and more accessible for a broader range of patients.
Behind the Scenes: What Inspired Us?
The idea for this innovative method emerged from practical challenges encountered in our clinical practice. When treating patients with delicate or loose teeth, the limitations and risks of DL-based techniques became glaringly apparent. Observing the potential harm of these traditional approaches led us to seek a solution that could mitigate these risks. Our goal was to create a procedure that would be effective and considerate of our patients' unique anatomical and dental vulnerabilities.
Why This Matters for the Community
Our work has important implications for both surgeons and patients. VACECs simplify the surgical process and reduce patient recovery time, making it a preferable option for treating ECs. Additionally, it provides a model for incorporating new technologies into routine practice, demonstrating the potential benefits of using advanced visualization and low-temperature ablation techniques.
By sharing this research on Springer Nature’s General & Internal Medicine and Surgery Community, we hope to encourage more discussions about integrating modern technologies in clinical settings. We also invite colleagues to share their experiences with innovative surgical techniques and how they address challenges in patient care.
Looking Forward
While VACECs has proven to be a successful alternative, there are always opportunities for improvement. Enhancing the image resolution of videolaryngoscopes and developing even more refined surgical tools could further increase the precision and applicability of this method. Future studies with larger patient populations could also provide more comprehensive data on long-term outcomes.
We are excited to see how our work will influence and inspire further advancements in minimally invasive laryngeal surgery. If you have thoughts or experiences related to this topic, we would love to connect and learn from each other.
Thank you for reading, and please share your feedback or join the conversation on Springer Nature’s Research Communities platform!
Follow the Topic
-
European Archives of Oto-Rhino-Laryngology

This is a distinguished international journal that publishes original clinical reports and clinically relevant experimental studies, as well as short communications presenting new results of interest in all specialties of Oto-Rhino-Laryngology and Head & Neck.


Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in