Diet switch pre-vaccination improves immune response and metabolic status in formerly obese mice
Published in Healthcare & Nursing, Microbiology, and Biomedical Research
Authors - Rebekah Honce, Ana Vazquez-Pagan, R. Chris Skinner, and Stacey Schultz-Cherry
Obesity is defined as a chronic disease by the Centers for Disease Control and Prevention. The increasing prevalence of obesity in the Western world has led to its correlation with a variety of diseases, with our group’s interest piqued after the 2009 H1N1 influenza virus pandemic. During this outbreak, obesity became widely regarded as a putative risk factor for hospitalization and death due to infection, with history repeating itself at the onset of the COVID pandemic1. Our lab, alongside others, dug into the molecular mechanisms underlying this association. Reports suggest obesity can alter influenza virus replication, immune responses and epidemiology in both mouse models and human cohorts2. We have also shown vaccination efficacy is reduced in mouse models of obesity3, which prompted the perennial question at every seminar, “what happens if the mice lose weight?”
Weight loss is often regarded as the catch-all solution for every health condition. However, the academic literature presents conflicting studies on obesity’s role as a risk or protective factor in influenza and other infectious diseases4,5, with contemporary research beginning to question obesity’s role in exacerbating or contributing to many chronic diseases. Thus, we felt we needed to similarly take a closer look at its association with viral infections, and simultaneously, answer some long-standing questions about diet change and vaccination. To do so, our study took the standard, diet-induced obese (DIO) mouse model, and after establishment of an obese phenotype as measured by body mass, switched the diet to standard chow to create four unique cohorts: always obese, formerly obese, always lean, and formerly lean. Our early studies found no improvement in survival if vaccination occurred while on the DIO protocol, regardless of weight loss post-vaccination.
After our initial findings suggested diet at the time of immunization was predictive of vaccine efficacy, we realized we needed some extra help to concretely define the mechanisms at play. Reaching out to our colleagues in the Thomas and McGargill Labs at St. Jude and the Skinner Lab now at the University of Vermont, we dug deeper into the immunological, metabolic, and immunometabolic features of our diet cohorts (Figure 1). We found dietary change was accompanied not only by weight loss but also a gradual improvement in molecular measures of metabolic health, namely serum leptin, adiponectin, and insulin. Further, at the time of vaccination, high-fat diet (HFD) exposure limited T-cell maturation leading to a prolonged state of activation and eventual poorer overall function at the time of recall (Figure 2). However, if vaccination occurred after HFD washout, we saw greatly improved survival outcomes at viral challenge. We next took a closer look at T-cell dynamics through immunophenotyping, functional immunostaining and extracellular flux analysis. Pre-vaccination diet switch reduced PD-1, CD98, and CD44hi expression across T-cell subsets, leading us to conclude switch from HFD to control had restored a more functional T-cell population (Figure 2).
Our study modeled weight gain and loss with a simple experimental design coupled with modern metabolomic techniques to mechanistically answer our central question in the context of rodent models of influenza vaccination and infection. However, in clinical settings, weight management is much more multifaceted, as weight is a complex interaction of genetic, epigenetic, socioeconomic, and environmental factors. Dieting is largely not sustainable and can cause additional stress to patients through either perceived personal failures or healthcare provider biases, leading to decreases in psychological and physical health6. While diet composition and quality does range widely across the world, increasingly we are observing high consumption of cheaply produced and ultra-processed foods, high in Calories, saturated fats and simple sugars, while being low in vitamins, minerals, and dietary fiber. This diet, dubbed the “Western diet,” has been implicated in rise in obesity and chronic disease rates. Yet disparities in healthcare access, economic and distance barriers to healthy food consumption, and monetization of physical activity have also abetted the observed rise. There is also pervasive fat bias in society and healthcare. Patients presenting with a larger body size are often not provided the necessary treatments—a key intervention to prevent influenza-related severe disease—thus promoting worse outcomes, although influenza-specific studies suggest patient obesity prompts quicker antiviral administration if healthcare is sought7.
Moreover, researchers and clinicians must remember malnutrition encompasses over- and undernutrition, with underweight status similarly associated with negative disease outcomes with influenza virus8. However, studies into undernutrition garner much less attention and research effort than those on overnutrition. Constant weight cycling and the accompanying metabolic fluxes can negatively impact the quality of the immune response yet are poorly studied in the context of viral infection9. Deeper investigations with refined diet designs should be applied to pre-clinical models to assess the complex interactions among dietary components, cellular metabolism, and host genetics. In clinical studies, moving away from a reliance on phenotypic observations, such as the body mass index as a measure of overall health10 and toward more labor-intensive but accurate metabolic measurements will improve our understanding of the broader metabolic syndrome and its effect on antiviral immunity.
In seeking to improve individual and public health or develop more effective treatments and preventatives for high-risk populations, we must consider societal, socioeconomic, genetic and individual barriers which prevent access to the textbook “healthy” lifestyle. Combating metabolic dysfunction is not just a personal health endeavor but must be accompanied through ensuring health equity by enacting societal-level interventions, anti-stigma campaigns in healthcare workers, and improved access to effective healthcare which will undoubtedly yield ripple effects in other realms of public health including infectious diseases. Our continued studies into immunometabolism and infectious diseases will also provide greater insight into the true causality of obesity-associated risks and help develop more effective therapeutic options for these and other high-risk populations.
References
- Caussy, C., Wallet, F., Laville, M. & Disse, E. Obesity is Associated with Severe Forms of COVID-19. Obesity 28, 1175 (2020). https://doi.org/10.1002/oby.22842
- Honce, R. & Schultz-Cherry, S. Impact of Obesity on Influenza A Virus Pathogenesis, Immune Response, and Evolution. Front Immunol 10, 1071 (2019). https://doi.org/10.3389/fimmu.2019.01071
- Karlsson, E. A. et al. Obesity Outweighs Protection Conferred by Adjuvanted Influenza Vaccination. Mbio 7 (2016). https://doi.org/10.1128/mBio.01144-16
- Biscarini, S. et al. The obesity paradox: Analysis from the SMAtteo COvid-19 REgistry (SMACORE) cohort. Nutrition, metabolism, and cardiovascular diseases: NMCD 30, 1920-1925 (2020). https://doi.org/10.1016/j.numecd.2020.07.047
- Pausé, C., Parker, G. & Gray, L. Resisting the problematisation of fatness in COVID-19: In pursuit of health justice. International Journal of Disaster Risk Reduction 54, 102021 (2021). https://doi.org/10.1016/j.ijdrr.2020.102021
- Tylka, T. L. et al. The weight-inclusive versus weight-normative approach to health: evaluating the evidence for prioritizing well-being over weight loss. Journal of Obesity 2014, 983495 (2014). https://doi.org/10.1155/2014/983495
- Segaloff, H. E. et al. The impact of obesity and timely antiviral administration on severe influenza outcomes among hospitalized adults. Journal of Medical Virology 90, 212-218 (2018). https://doi.org/10.1002/jmv.24946
- Moser, J. S. et al. Underweight, overweight, and obesity as independent risk factors for hospitalization in adults and children from influenza and other respiratory viruses. Influenza Other Respir Viruses 13, 3-9 (2019). https://doi.org/10.1111/irv.12618
- Cottam, M. A., Itani, H. A., Beasley, A. A. & Hasty, A. H. Links between Immunologic Memory and Metabolic Cycling. The Journal of Immunology 200, 3681-3689 (2018). https://doi.org/10.4049/jimmunol.1701713
- Egom, E. E. et al. Time to redefine body mass index categories in chronic diseases? Spotlight on obesity paradox. International journal of food sciences and nutrition 69, 513-523 (2018). https://doi.org/10.1080/09637486.2017.1389859
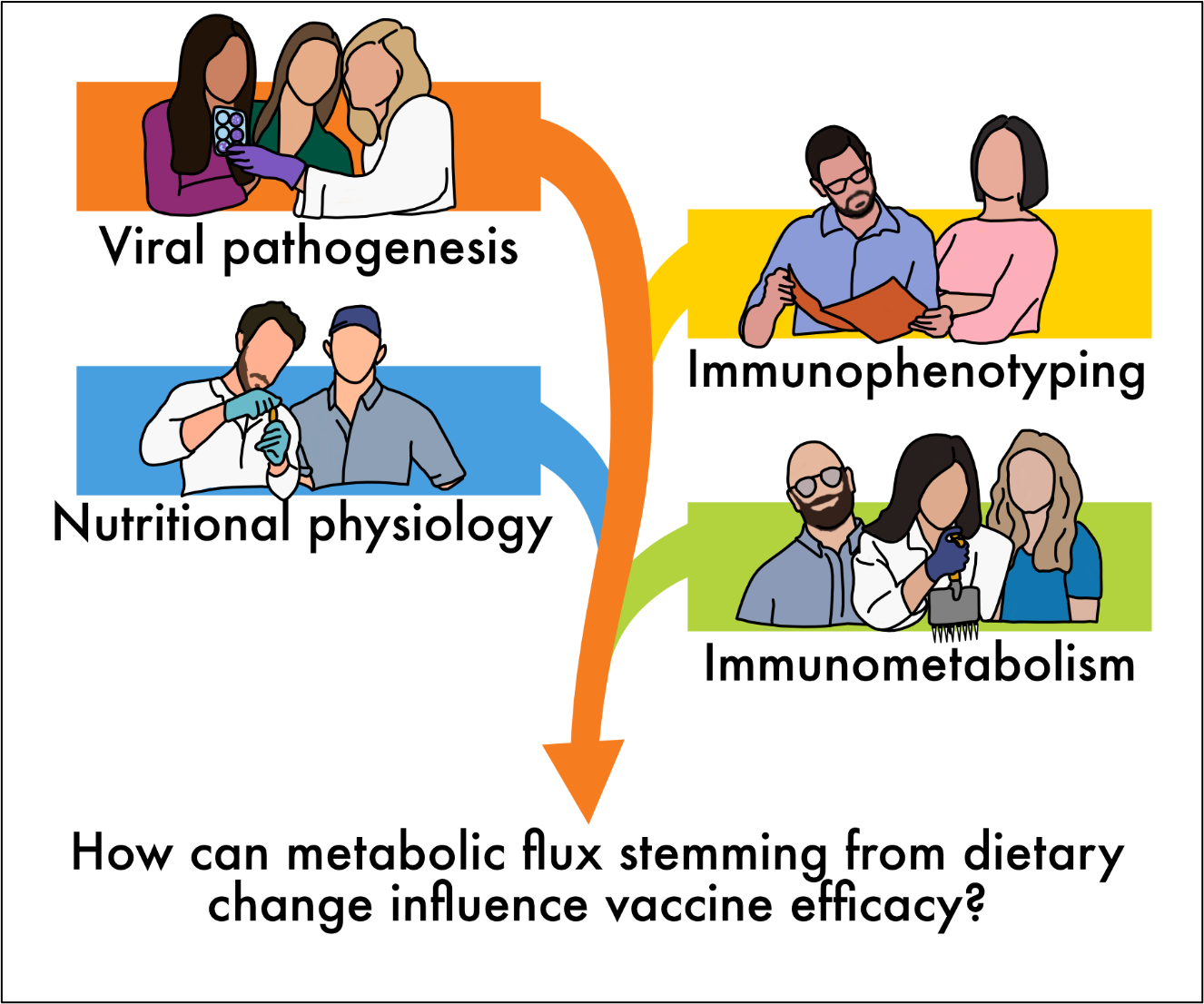
Figure 1. Cross-discipline efforts to answer our central research questions.n
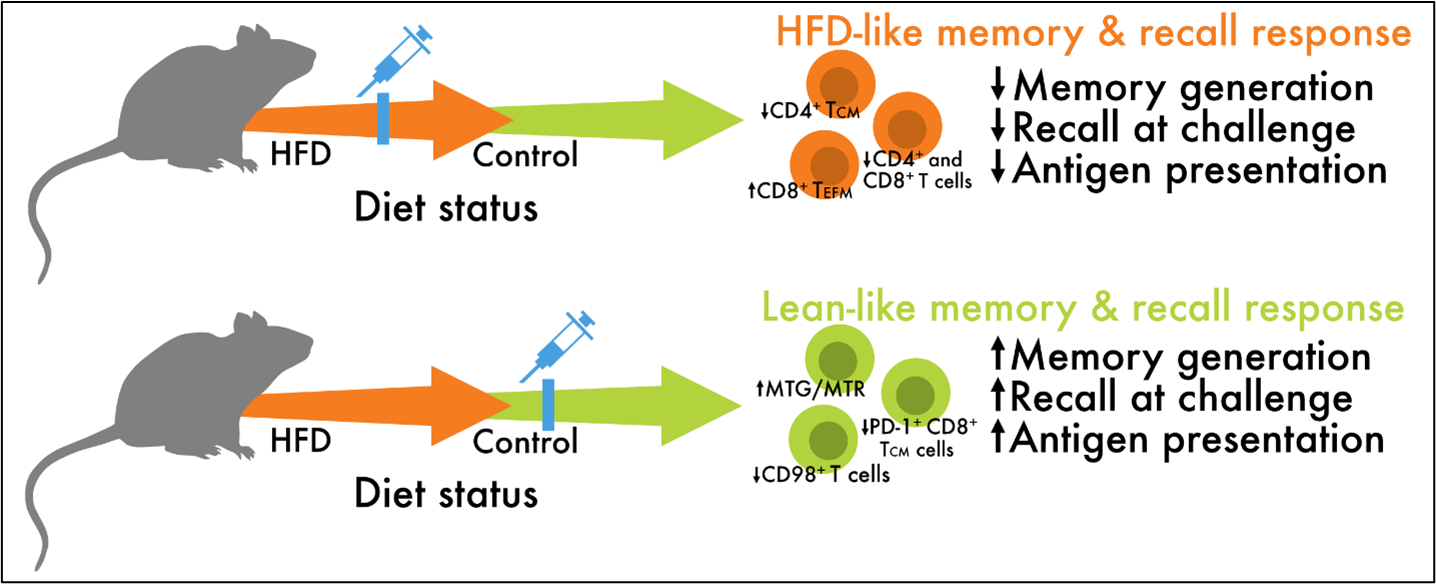
Figure 2. Memory and recall responses are sensitive to diet at the time of vaccination.
Follow the Topic
-
Nature Microbiology

An online-only monthly journal interested in all aspects of microorganisms, be it their evolution, physiology and cell biology; their interactions with each other, with a host or with an environment; or their societal significance.
Related Collections
With Collections, you can get published faster and increase your visibility.
The Clinical Microbiome
Publishing Model: Hybrid
Deadline: Mar 11, 2026



Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in