Effect of Stress Management Based Self-Care Counseling on Glycemic Control in Women with Gestational Diabetes Mellitus: A Randomized Controlled Trial Study
Published in Biomedical Research, Behavioural Sciences & Psychology, and Arts & Humanities
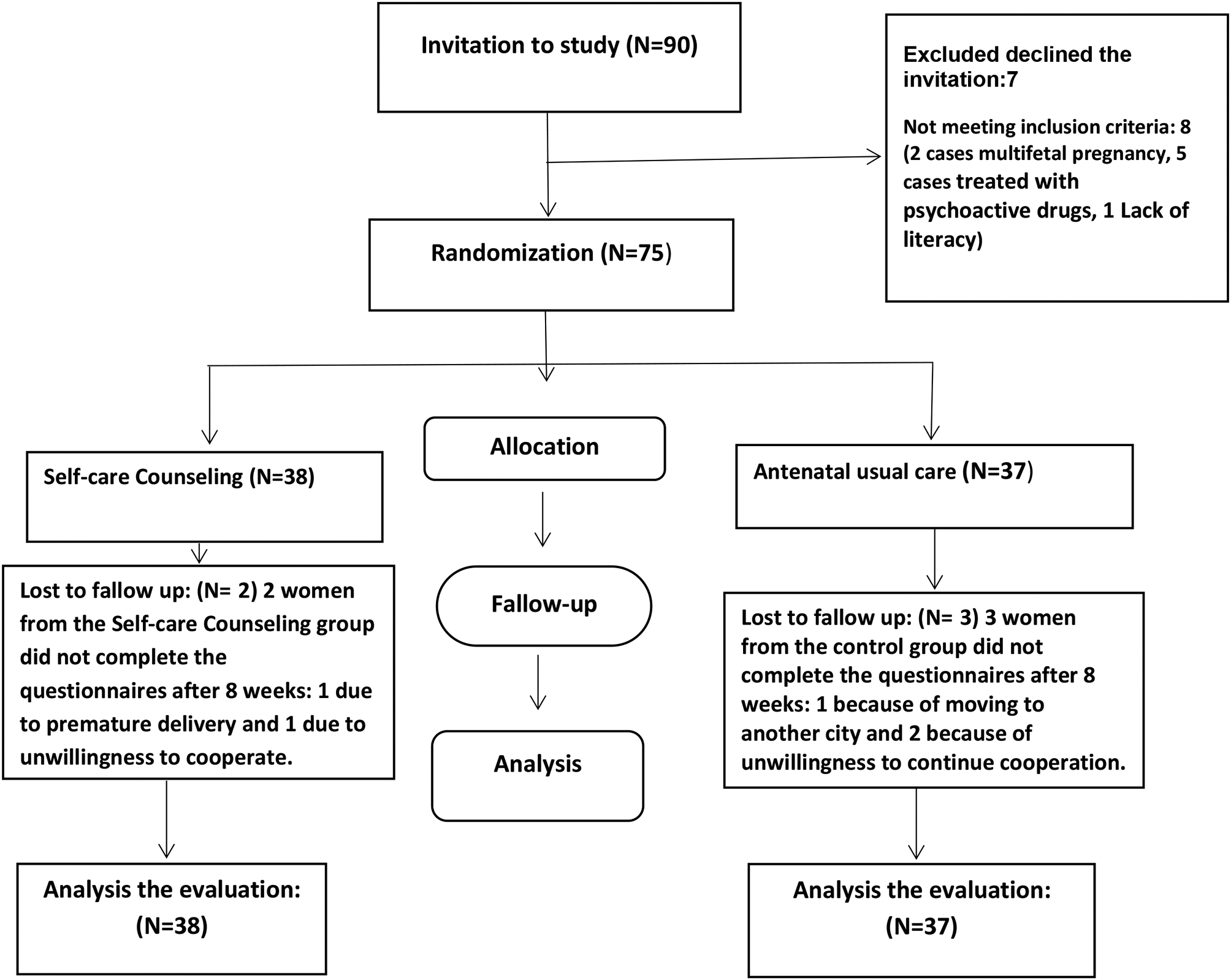
In this randomized controlled trial, participants included pregnant women diagnosed with gestational diabetes, who were divided into two groups: the experimental group and the control group. The experimental group received self-care counseling based on stress management, while the control group only received standard care.
Researchers used tools to assess blood sugar levels, stress management techniques, and the quality of life of participants. These measurements were conducted before and after the counseling period to evaluate the program's impacts.
The results of this study showed that women in the experimental group had a significant reduction in their blood sugar levels. Additionally, their quality of life and sense of satisfaction improved. Researchers found that stress management counseling can help reduce stress and anxiety in pregnant women, leading to better blood sugar control.
Given that stress can negatively affect blood sugar management, considering mental health alongside physical health is crucial. Pregnant women who experience less stress and anxiety generally cope better with the challenges of gestational diabetes.
Based on the findings of this study, the researchers suggest that similar programs could be considered as part of the standard treatment for women with gestational diabetes. This study not only highlights the importance of psychological counseling and self-care education but also represents a significant step toward improving the quality of life for pregnant women with gestational diabetes.
Researchers hope that this study can facilitate health and treatment policies concerning gestational diabetes.
Follow the Topic
-
BMC Pregnancy and Childbirth

This is an open access, peer-reviewed journal that considers articles on all aspects of pregnancy and childbirth. It welcomes submissions on the biomedical aspects of pregnancy, breastfeeding, labor, maternal health, maternity care, trends and sociological aspects of pregnancy and childbirth.
Your space to connect: The Psychedelics Hub
A new Communities’ space to connect, collaborate, and explore research on Psychotherapy, Clinical Psychology, and Neuroscience!
Continue reading announcementRelated Collections
With Collections, you can get published faster and increase your visibility.
Fetal and placental surgery
BMC Pregnancy and Childbirth is calling for submissions to our Collection on Fetal and placental surgery.
Fetal and placental surgery represents a rapidly evolving field that aims to address congenital anomalies and complications during pregnancy through in-utero interventions. These surgical techniques, which can include procedures such as fetoscopy and placental surgery, enable clinicians to treat conditions that may adversely affect fetal development, health, and survival. Placental surgery encompasses a variety of interventions, including but not limited to, the treatment of placental insufficiency, the management of placenta previa, and the correction of placental vascular anomalies. As technology and surgical techniques advance, this area of medicine continues to expand, offering promising new avenues for intervention that can significantly enhance neonatal outcomes.
The Collection invites researchers and clinicians in fields including maternal-fetal medicine, obstetrics and obstetrical surgery, and neonatology, to contribute research that explores topics including, but not limited to, in-utero surgical techniques, emergency obstetric practices, recent advancements in minimally invasive techniques, and outcomes associated with these interventions.
All manuscripts submitted to this journal, including those submitted to collections and special issues, are assessed in line with our editorial policies and the journal’s peer review process. Reviewers and editors are required to declare competing interests and can be excluded from the peer review process if a competing interest exists.
Publishing Model: Open Access
Deadline: Jun 10, 2026
Respectful maternity care - Part II
BMC Pregnancy and Childbirth is calling for submissions to our Collection on Respectful maternity care - Part II.
The World Health Organization defines respectful maternity care (RMC) as care that maintains dignity, privacy, and confidentiality of pregnant and birthing women, ensures freedom from harm and mistreatment, and enables informed choice and continuous support during labor and birth. RMC is considered a fundamental human right. Despite the acknowledged importance of providing RMC to all women, many women still experience disrespect and abuse during labor and birth across global contexts.
BMC Pregnancy and Childbirth is calling for submissions on ‘Respectful maternity care’ to bring together research on the benefits of respectful maternity care and the challenges in its implementation, both at the provider level and the system level. Both qualitative and quantitative research are welcome. Topics of interest include, but are not limited to, prevalence of disrespect and abuse in maternity care, implementation of respectful maternity care, RMC and maternal and neonatal outcomes, interventions to enhance and promote RMC, RMC in postnatal care, and effective communication and informed choice.
All manuscripts submitted to this journal, including those submitted to collections and special issues, are assessed in line with our editorial policies and the journal’s peer review process. Reviewers and editors are required to declare competing interests and can be excluded from the peer review process if a competing interest exists.
All manuscripts submitted to this journal, including those submitted to collections and special issues, are assessed in line with our editorial policies and the journal’s peer review process. Reviewers and editors are required to declare competing interests and can be excluded from the peer review process if a competing interest exists.
Publishing Model: Open Access
Deadline: Aug 12, 2026



Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in