Exploring Digital Musculoskeletal Care as an Avenue to Build Health Equity
Published in Healthcare & Nursing and Pharmacy & Pharmacology

Context
The advent of digital health has opened up a series of new possibilities for healthcare. Several studies have shown how digital health can alleviate time and geographical barriers to accessing care. However, those are not the only barriers to achieving good health outcomes, particularly when it comes to musculoskeletal (MSK) pain. Non-medical factors such as income, education, job security, housing, social inclusion, and access to healthcare services can account for 30-55% of health outcomes. Collectively, these factors have been described as Social Determinants of Health (SDOH). Developing effective digital care pathways requires careful consideration of SDOH and a whole-person approach.
Delivering patient-centered and culturally-appropriate care in a digital setting
Research has shown that engagement can be maximized through shared decision-making and effective communication channels between patients and healthcare professionals. To answer these needs, we developed our programs in a way that ensured each patient was viewed holistically and empowered early in the program, beginning by establishing treatment goals through shared decision-making. In addition, multiple communication channels were available to patients and physical therapists to guarantee continued support and motivation.
Research also shows that satisfaction and trust are enhanced when patients from underrepresented groups or ethnicities share similar cultural or ethnic backgrounds with their health professionals. As such, Sword invested in a diverse and culturally-sensitive clinical care team, including professionals from seven racial/ethnic backgrounds, covering five languages, and provided cultural competence training to all professionals. In addition, to foster an easier and stronger therapeutic alliance, we enabled patients to choose their therapist from this diverse pool of doctors of physical therapy.
How this prompted research
Our own research had pointed to the linkage between specific SDOH factors and poorer health outcomes at baseline. In prior studies, we assessed whether we were able to assist patients independently of their geographical location (either urban or rural), and independently of their race/ethnicity. These studies found that this digital health program was promoting positive outcomes regardless of baseline characteristics. These valuable insights seemed to point towards a potential to promote health equity. Given the scarce literature on the potential influence of digital health in addressing a broader spectrum of SDOH we believed our contribution could be particularly meaningful to diminishing this literature gap. The unanswered question was whether the specific design of this digital care program would positively impact patient outcomes, regardless of each patient's wide context, and potentially help to change the landscape.
Designing the Study
To be able to evaluate the impact of our digital care programs in the several domains that were required (age, demographics, race/ethnicity, income, education, employment status, housing, transportation, rurality, proximity to healthcare facilities) we had to expand the information that we collected directly through study surveys. To that effect, we used validated metrics derived from the U.S. census bureau for rurality (rural-urban commuting area/RUCA scores) and social deprivation (Social deprivation index/SDI), and we cross-referenced each patient zip code with a publically available dataset with county-level geographic distribution of healthcare resources (https://healthsites.io/). Then, we applied a multiple-group latent growth curve analysis to understand outcome change behavior of five categories of SDI with increasing social deprivation (C1-C5).
Study Results
We studied a cohort of 12,062 patients with self-reported chronic MSK pain, spread throughout the entire U.S. Ten percent of the population belonged to the more socially deprived category (C5)(Figure 1). As previously documented, we observed SDOH were having a significant toll on the baseline outcomes of these patients (Figure 2). Indeed, categories associated with higher social deprivation (C4 and C5) were the ones reporting worse outcomes at baseline with an increasing trend clearly observable from category to category.
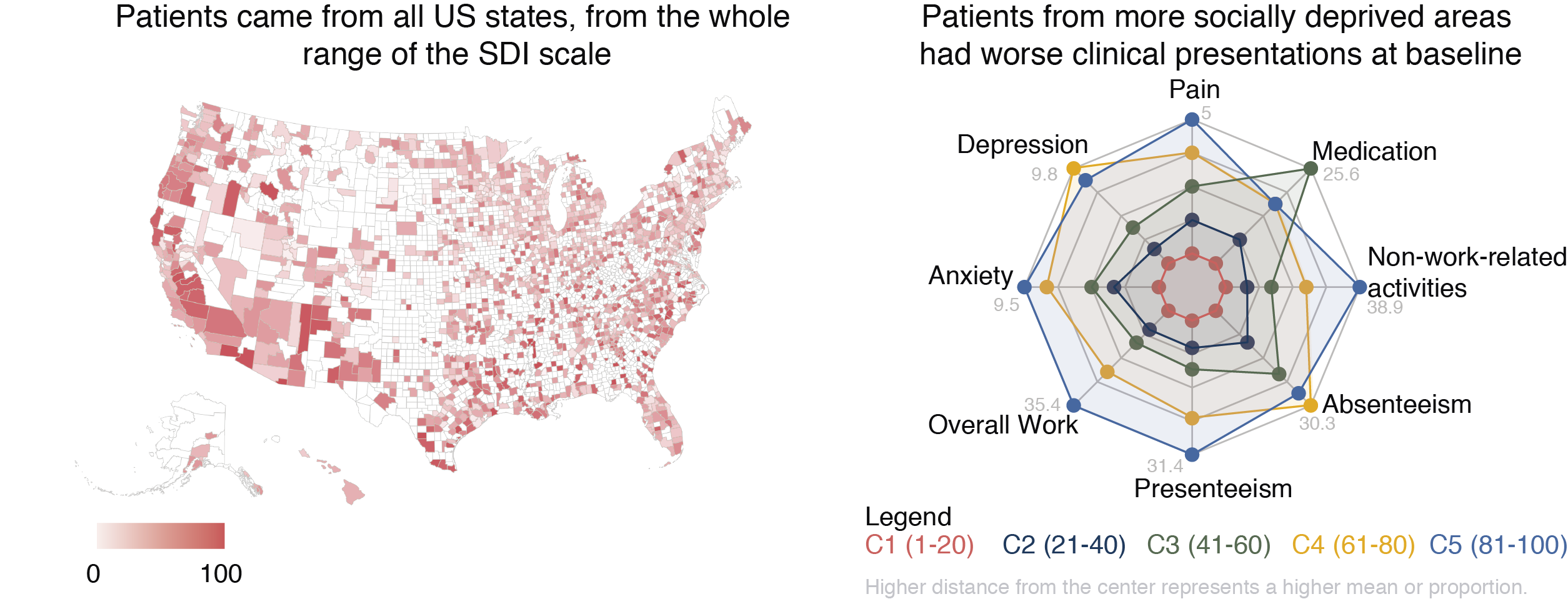
In this cohort, the majority of the patients in the more vulnerable socioeconomic category (C5) resided in urban locations, which might explain their increased proximity to healthcare facilities. However, proximity did not equate to less aggravated outcomes at baseline. This result alone highlights the pertinence of researching the other contributors for health outcomes, and exploring solutions that tackle the multiple barriers these patients face.
When analyzing the longitudinal results of the different outcomes, we observed that patients, regardless of their socioeconomic background, race, or even proximity to healthcare facilities, were able to achieve significant improvements in all studied outcomes (pain, analgesics intake, mental health, and productivity). In fact, patients who were identified as more socially deprived achieved better productivity outcomes than those who were not.
Expectations for the Future
This study has provided new insights in regards to the ability of digital care programs to reach and engage individuals from all socioeconomic levels, and in deploying effective care that results in improved outcomes irrespective of backgrounds. It is our belief that this and other studies—by our group and many others—may help to pave the way to a more generalized adoption of digital care pathways, as a way to provide effective care in a more affordable and scalable way. It is our hope that digital health can help reduce inequalities in healthcare.
Follow the Topic
-
npj Digital Medicine

An online open-access journal dedicated to publishing research in all aspects of digital medicine, including the clinical application and implementation of digital and mobile technologies, virtual healthcare, and novel applications of artificial intelligence and informatics.
Related Collections
With Collections, you can get published faster and increase your visibility.
Digital Health Equity and Access
Publishing Model: Open Access
Deadline: Mar 03, 2026
Evaluating the Real-World Clinical Performance of AI
Publishing Model: Open Access
Deadline: Jun 03, 2026





Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in