Exploring the potential of self-managed organizational structure in enhancing home-based healthcare services in India
Published in Public Health, Behavioural Sciences & Psychology, and Business & Management
Inception: Where the idea began
The seed for this research was sown during my doctoral journey in Organizational Behavior, where I was studying person–environment fit and self-management in organizations. Around the same time, I began observing India’s healthcare system closely — especially how the COVID-19 pandemic exposed its structural fragilities and human costs. The contrast between overburdened hospitals and the growing need for dignified, home-based care led to a critical question:
Could the principles of self-managed organizations offer a sustainable model for homecare in India?
Discovering global models of decentralized, nurse-led care in the literature was an eye-opening moment. These systems thrived on autonomy, trust, and collaboration — the very principles I was exploring theoretically. The possibility of applying such ideas to India’s healthcare context felt both bold and necessary.
Conceptual grounding and research direction
The next step was to find an Indian context where self-management principles were being applied in healthcare. Observing such a system in practice provided a living example of how decentralized structures operate without rigid hierarchies, allowing frontline professionals the freedom to make real-time decisions. This became an ideal setting to study how organizational design influences care outcomes and employee engagement.
To frame the research theoretically, we linked self-management to Peter Senge’s learning organization framework, finding deep resonance with its emphasis on continuous learning, shared vision, and systems thinking — all vital to adaptive healthcare systems.
The research process: entering the field
The empirical journey was both intellectually stimulating and logistically demanding. We conducted in-depth semi-structured interviews with twelve management members over a two-year period. These conversations offered rich insights into autonomy, teamwork, conflict resolution, and the cultural adaptations required for self-management in the Indian context.
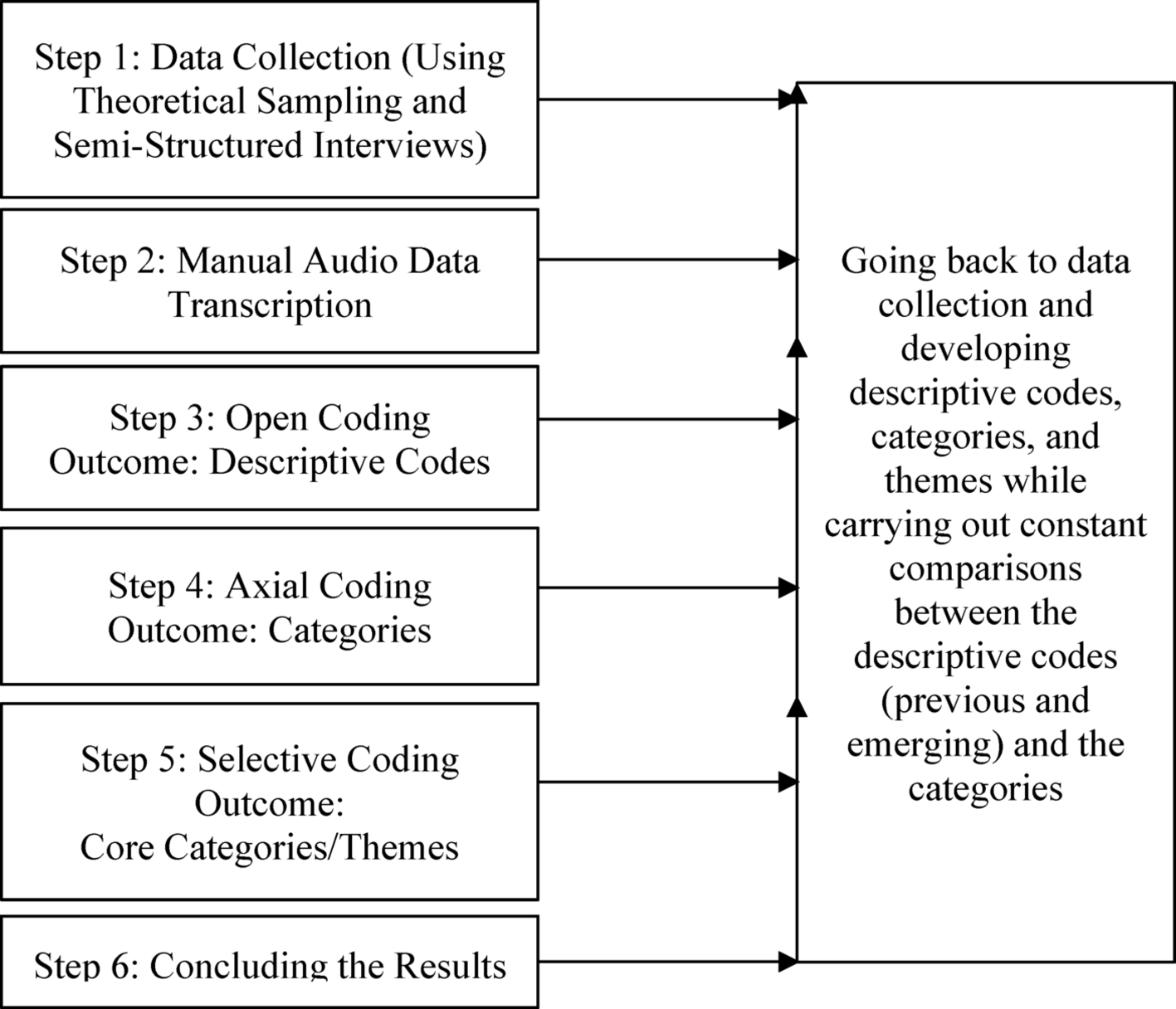
Following Constructivist Grounded Theory (CGT), we allowed findings to emerge organically. Each round of analysis revealed new layers — from trust and empowerment to communication and coordination. The iterative process of coding, comparing, and refining themes was as humbling as it was enlightening.
Challenges and learning moments
One of the biggest challenges was gaining access and building trust within a self-managed system. With no single gatekeeper, establishing rapport required patience, empathy, and respect for participants’ professional rhythms.
Another challenge lay in maintaining reflexivity. Coming from management and psychology backgrounds, we had to ensure our interpretations reflected participants’ lived realities rather than academic assumptions. Translating these nuanced experiences into theoretical insights demanded both rigor and humility.
Insights that stayed with us
Two key themes emerged:
-
Creating a nurturing work environment built on trust, collaboration, and empowerment.
-
Enhancing communication and coordination through both technology and human connection.
These are not merely organizational traits — they are human foundations for sustainable care. When professionals are trusted and supported, patient satisfaction and care quality naturally improve.
Reflections and looking forward
Writing this paper deepened our belief that organizational structures are moral systems — shaping how people relate, decide, and care. In India’s largely hierarchical healthcare landscape, self-management offers a humane and adaptive alternative that balances autonomy with accountability.
This journey reaffirmed that research is not only about discovering models but also about re-discovering human potential within them. We hope this work inspires healthcare leaders and policymakers to view self-management not as a borrowed concept, but as a universal principle rooted in trust, respect, and shared purpose.
Follow the Topic
-
Discover Health Systems

This journal takes a multidisciplinary approach to address systems-level research and discussions relating to health systems, services and informatics, reflecting health outcomes, including from business and health policy perspectives.
Related Collections
With Collections, you can get published faster and increase your visibility.
Building Resilient Health Systems and Outbreak Preparedness in Africa: Policy, Governance, and Technological Innovation
Achieving timely prevention, detection, and response to infectious disease threats, while maintaining equitable access to essential services—depends on robust, well-governed health systems. In Africa’s diverse contexts, strengthening these systems requires integrated policy frameworks, adaptive management practices, and innovative technologies that address gaps in surveillance, workforce capacity, supply chains, and community engagement.
This Article Collection examines multidisciplinary strategies to enhance health system resilience and epidemic preparedness across the continent. We focus on:
- Policy and Governance: Crafting adaptive national and subnational policies, financing models, and regulatory environments that incentivize rapid outbreak response and sustain routine care.
- Health System Management: Optimizing human resources for health, supply-chain logistics, and facility-level coordination to maintain continuity of care during emergencies.
- Digital Health & Informatics: Deploying electronic surveillance platforms, mobile health (mHealth) tools, and data-analytics dashboards for real-time monitoring, early warning, and evidence-based decision-making.
- Surveillance & Laboratory Networks: Expanding laboratory capacity, sample-transport systems, and integrated One Health approaches to detect zoonoses and emerging pathogens.
- Community Engagement & Risk Communication: Leveraging regional partnerships, local governance, and culturally tailored messaging to build trust and promote preventive behaviors.
- Operational Research & Evaluation: Implementing outbreak simulations, performance metrics, and rapid-cycle evaluations to refine interventions and inform scalable best practices.
We welcome submissions that generate practical, scalable solutions for African health systems. By uniting insights from policymakers, health managers, informaticians, and frontline practitioners, this Collection aims to inform evidence-driven investments, strengthen preparedness capacities, and improve health outcomes across the continent.
Publishing Model: Open Access
Deadline: Jun 01, 2026
Advances in Large Language Models for Health Systems
This collection invites original research articles, reviews, and case studies at the intersection of Computational Intelligence (CI), Artificial Intelligence (AI), and healthcare informatics and healthcare records, with a focus on Large Language Models (LLMs) methods and architectures. The aim is to showcase innovative methodologies and applications that bridge cutting-edge CI techniques with real-world challenges in healthcare.
We welcome contributions that present novel algorithms, frameworks, and applications of AI and CI in areas such as, clinical decision support, healthcare informatics, and ethical or legal aspects of medical AI. Special attention will be given to interdisciplinary work that highlights translational potential, system-level integration, or demonstrates real-world deployment within health systems. This collection seeks to foster collaboration among researchers, clinicians, data scientists, and system designers to promote advances that will shape the future of intelligent health technologies.
Topics of Interest Include, but Are Not Limited To:
- Integration of LLMs with electronic health records (EHRs) and clinical decision support systems
- Ethical, legal, and regulatory considerations in deploying LLMs in healthcare
- Case studies demonstrating real-world implementation of LLMs in health systems
Any study solely on development of an LLM application in healthcare records maintenance or health informatics should have application analysis to support.
Keywords: Computational Intelligence, Artificial Intelligence, Large Language Models, Healthcare Informatics, Clinical Decision Support, Intelligent Medical Systems。
Publishing Model: Open Access
Deadline: Apr 04, 2026
Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in