Failure of Biomarkers in Extracellular Vesicles for Parkinson's disease and Related Disorders Diagnosis
Published in Neuroscience
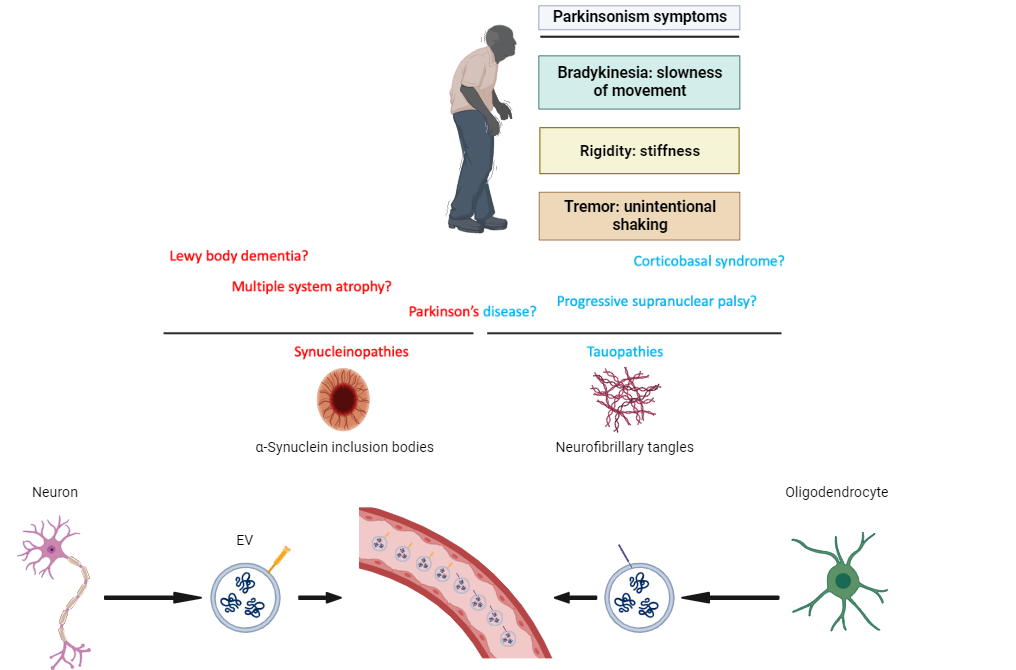
Parkinsonian disorders are a group of neurological conditions that primarily affect a person’s movement, causing symptoms like tremors, stiffness, and slowness of movement. The most well-known of these is Parkinson's disease, which is caused by the loss of nerve cells in a part of the brain called the substantia nigra. These cells produce dopamine, a chemical that helps control body movement. The same condition that affected Muhammad Ali, one of the greatest boxers of all the time. However, Parkinsonian disorders encompass more than just Parkinson's disease. They include multiple system atrophy, dementia with Lewy body, progressive supranuclear palsy, and corticobasal degeneration. Each of these disorders has unique characteristics, but they share the common challenge of disrupted motor functions and often overlap in symptoms, making diagnosis and treatment a complex task.
Extracellular vesicles (EVs) have emerged as a potential source of biomarkers, carrying cell-state-specific messages that reflect the status of their parent cells. These tiny vesicles can traverse the blood-brain barrier (BBB), offering a glimpse into the cellular activities within the central nervous system (CNS). This unique ability positions them as promising candidates for diagnosing Parkinsonian disorders. Researchers are intrigued by the possibility that EVs might contain specific markers indicative of these disorders, potentially revolutionizing early detection and monitoring.
However, this hypothesis faces significant challenges. EVs can be uptaken and recycled by other cells, complicating their interpretation. Even if they originate from the CNS, their content might not accurately reflect the current state of the brain due to this recycling and uptake by different cell types. This raises critical questions about the reliability of EVs as mirrors of CNS conditions. Can they truly be used for biomarker discovery in Parkinsonian disorders, or do they present a misleading picture? To address these uncertainties, a comprehensive meta-analysis was conducted. The findings from this study provide essential insights, potentially reshaping our understanding of the role of EVs in diagnosing these complex neurological conditions
The meta-analysis embarked on an extensive evaluation of what are often referred to as speculative CNS-enriched extracellular vesicles, in the context of Parkinsonian disorders. By encompassing all studies available to date, it aimed to determine if these vesicles could reliably distinguish between various Parkinsonian conditions and healthy controls. However, the outcome of this analysis indicated that these CNS-enriched markers found within extracellular vesicles fell short of expectations. They did not consistently differentiate between the disorders or in comparison with healthy individuals, casting doubt on their touted potential as diagnostic tools. This finding is critical, especially considering the challenges of publication bias, where results favoring positive outcomes are more likely to be reported. Furthermore, the analysis uncovered a significant degree of heterogeneity across the studies, with variances in experimental approaches and patient populations. These factors collectively contribute to the skepticism surrounding the speculative CNS-enriched extracellular vesicles as effective biomarkers for Parkinsonian disorders, prompting a reevaluation of their role and utility in diagnosis.
The findings from the comprehensive meta-analysis send a clear message to the scientific community and public funding bodies: it's time to redirect efforts and resources. The pursuit of speculative CNS-enriched extracellular vesicles as biomarkers for Parkinsonian disorders, despite initial promise, has not yielded the expected breakthroughs. Continued investment in this area seems less likely to benefit patients with these disorders. Therefore, researchers and funding agencies should consider pivoting towards more promising avenues of investigation. Exploring alternative biomarkers or novel therapeutic strategies could offer more tangible hope and assistance to those affected by Parkinsonian disorders. This strategic shift in focus and allocation of resources is not just a scientific imperative but a moral one, ensuring that the primary goal remains the improved understanding, diagnosis, and treatment of these complex and debilitating conditions.
Follow the Topic
-
Journal of Neurology

Journal of Neurology is a peer-reviewed international journal focused on all aspects of clinical neurology from diagnosis to treatment.


Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in
Check out the other part of the meta-analysis here!
https://doi.org/10.1002/jex2.121