Guidance on writing about health inequality
Published in Social Sciences, Public Health, and Arts & Humanities
Background
In the 2024 World Health Organization (WHO) book Health inequality monitoring: harnessing data to advance health equity, WHO Director General Dr Tedros Adhanom Ghebreyesus references the role of monitoring health inequalities for “moving towards a world in which health is not a luxury for some, but a right for all.”
By identifying, measuring and tracking inequalities in health between population groups that are socially advantaged or disadvantaged, we can better understand where health gaps exist. And, with this knowledge, we can start to imagine how policies, programmes and practices – both within the health sector, and beyond – can be designed to enable everyone the opportunity for a good standard of health.
Our article Writing about health inequality: recommendations for accurate and impactful presentation of evidence, published in the International Journal for Equity in Health, provides guidance on the presentation of health inequality analyses through written reports. It aims to bring together best practices for writing about health inequality, and to shed light on common pitfalls. The article addresses a broader aspiration of effectively using evidence about health inequalities to inform actions for more equitable health systems.
What was our focus?
Through our article, we wanted to address certain technical aspects of writing, such as word choices, statistical content, and metadata. We call this section of the article the “micro” aspects of writing. We devote the following section of the article to “macro” issues regarding the structure and completeness of written reports. We then acknowledge considerations related to inclusivity and respect that arise when writing addresses the situation of populations that are traditionally disadvantaged in society. This “meta” section of the article discusses the use of affirming language, strength-based messaging and engaged writing processes.
We were fortunate to develop this article alongside a group of devoted coauthors, who represent a range of disciplinary, professional and geographical environments. This diversity of perspectives, together with the broad selection of literature that we consulted in developing the article, revealed rich discussions about the different traditions around health inequality evidence and reporting practices. The guidance in this article aims to attend to these differences – acknowledging them and reconciling them where possible. For example, on the matter of defining health inequality and health inequity, we wrote:
Inconsistencies in the meanings attached to labels for health differences contribute to fragmentation of this field of research. It is outside the scope of this paper to resolve these debates or offer definitive guidance on the use of terminology. Rather, in the absence of a clear consensus, we recommend the use of language that best reflects the customary usage and preferences of the target audiences, and that terminology always be clearly defined and used consistently.
Benefits of common guidance
In the article, we highlight several advantages of developing and adopting common guidance for writing about health inequality analyses. Standard terminology and protocols for presenting health inequality evidence promotes greater accessibility of evidence across disciplines. This reduces fragmentation in the field and fosters enhanced knowledge sharing and collaboration. Further, adopting common approaches to reporting strengthens the possibilities for knowledge synthesis activities (e.g. literature reviews and meta-analyses), which are of increasing relevance given the growing output of health inequality research.
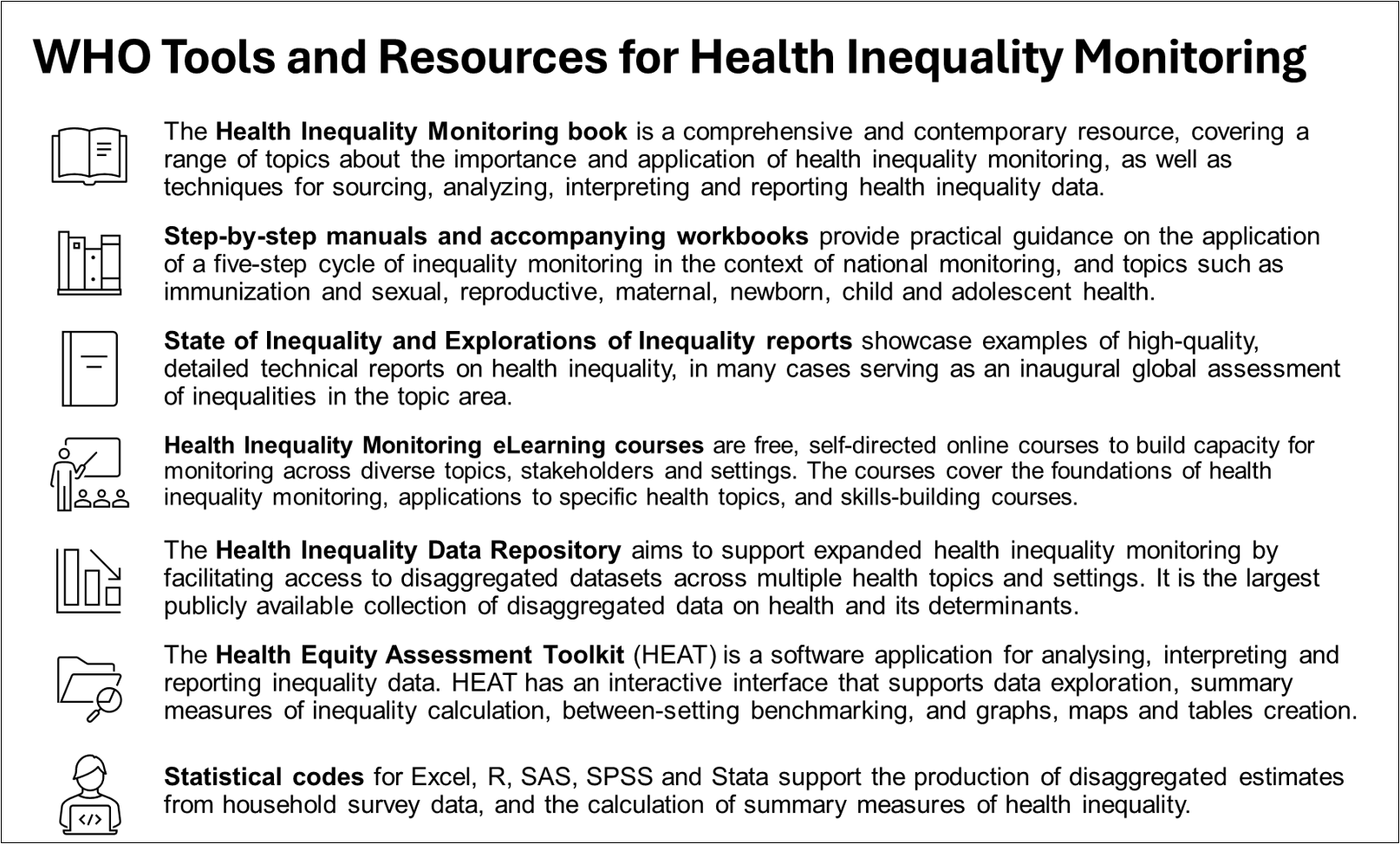
Practically, however, standardized approaches require flexibility to adapt to the contexts in which they are applied. Together with other colleagues in the WHO Health Inequality Monitoring Team, we have developed of a series of tools and resources – some of which are mentioned in the article – for the major components of health inequality monitoring. They are premised on a standardized, yet flexible, approach for global, national and subnational level inequality monitoring, and are publicly available through the WHO Health Inequality Monitor.
Forthcoming initiatives
In preparing this article, we opted for a focused scope on writing about health inequalities. We acknowledge, however, that written outputs (and other forms of communication) often also present data in a variety of other ways, such as graphs, maps, tables and interactive dashboards. To expand the evidence base on these topics, some of the coauthors have developed a companion article on inequality data visuals. It discusses considerations for the selection and design of graphs and maps frequently used for reporting health inequality analyses. This companion article is currently under review.
Wider efforts to expand and promote health inequality monitoring are underway by the Health Inequality Monitoring Network, which was launched in June 2025. The Network aims to advocate for enhanced health inequality monitoring globally, regionally, nationally and sub-nationally, and supports the scale up of the WHO activities in this area.
Disclaimer: The authors are affiliated with the World Health Organization. The authors alone are responsible for the views expressed in this article and they do not necessarily represent the decisions, policy or views of the World Health Organization.
Follow the Topic
-
International Journal for Equity in Health

This journal presents evidence relevant to the search for, and attainment of, equity in health across and within countries and publishes research which improves the understanding of issues that influence the distribution of health and healthcare within populations.
Related Collections
With Collections, you can get published faster and increase your visibility.
Racism and Health
The ongoing advancement of our understanding of how racism impacts health - both directly and structurally - is crucial for addressing the deep-rooted health inequities that persist globally. Structural racism shapes health outcomes among racialized populations, contributing to inequities in healthcare access and quality, and impacting social, political, or environmental determinants of health. Existing research also connects direct and visible manifestations of racism, such as major and everyday discrimination, to negative health outcomes. At the same time, racism does not operate in isolation. A growing body of research shows how it intersects with other systems of oppression—such as classism and patriarchy—and with broader social determinants of health, producing compounded and context-specific inequities. An intersectional lens is therefore essential to understand how overlapping structures of power and exclusion shape health and healthcare experiences. These insights are essential in conducting rigorous and thorough health research, guiding anti-racist health policy, and ultimately, ensuring equitable health for all.
Looking forward, research holds the potential to develop new methodologies and indices and unveil complexities in how racism manifests within healthcare systems and societal structures. By deepening our collective understanding, we can develop more effective interventions that target the root causes of health inequities.
We invite researchers to contribute to this special Collection on Racism and Health, focusing on advancing our understanding and addressing health inequities. Topics of interest include but are not limited to:
- Racism as a structural determinant of health
- Racism as a direct determinant of health
- Racialized health outcomes in different populations
- Intersectionality and inequities in health, healthcare access and quality
- Nexuses between social, political, and environmental determinants of health and systemic discrimination
- Anti-racist health policy frameworks and systems
- Impact of racism on mental health
- Health inequities in reproductive, maternal, and child health
- Obstetric and reproductive violence
- Community-based interventions for equitable health
- Decolonizing health research and global health epistemologies
We strongly encourage contributions from racialized scholars and authors with lived experience or expertise in addressing systemic discrimination in health research.
This Collection supports and amplifies research related to SDG 3, Good Health and Well-Being and SDG 10, Reduced Inequalities.
All submissions in this collection undergo the journal’s standard peer review process. Similarly, all manuscripts authored by a Guest Editor(s) will be handled by the Editor-in-Chief. As an open access publication, this journal levies an article processing fee (details here). We recognize that many key stakeholders may not have access to such resources and are committed to supporting participation in this issue wherever resources are a barrier. For more information about what support may be available, please visit OA funding and support, or email OAfundingpolicy@springernature.com or the Editor-in-Chief.
Publishing Model: Open Access
Deadline: Aug 14, 2026
Mental Health Inequities in Crisis: Insights from South-East Asia
The importance of advancing our collective understanding of mental health disparities during extraordinary crises, particularly in South-East Asia, cannot be overstated. As the region faces a multitude of challenges—ranging from natural disasters to public health emergencies—there is a pressing need to explore the variations in mental health impacts across different communities. Significant strides have been made in this area, including the identification of specific risk factors, the implementation of culturally sensitive interventions, and the recognition of mental health as a critical component of overall well-being. However, much work remains to be done. Future research has the potential to uncover new insights into the social determinants of mental health, enhance intervention strategies, and inform policies that promote equity. By deepening our understanding of these issues, we can better address the unique mental health challenges faced by vulnerable populations in the region.
We welcome all article types, including original research, reviews, meta-analyses, and perspectives.
We invite researchers to contribute to this special Collection. Topics of interest include but are not limited to:
-Socioeconomic & Geographic Disparities in Mental Health Access
-Community-Level Heterogeneity in Mental Health Outcomes
-Social Determinants of Mental Health in Crisis Contexts
-Culturally Adapted Mental Health Interventions
-Youth Mental Health in Crisis: Vulnerability and Resilience
-Gender and Mental Health: Differential Impacts and Responses
-Stigma, Barriers, and Facilitators to Mental Health Care
-Digital Mental Health Innovations in Low-Resource Settings
This Collection supports and amplifies research related to SDG 3, Good Health and Well-Being.
All submissions in this collection undergo the journal’s standard peer review process. Similarly, all manuscripts authored by a Guest Editor(s) will be handled by the Editor-in-Chief. As an open access publication, this journal levies an article processing fee (details here). We recognize that many key stakeholders may not have access to such resources and are committed to supporting participation in this issue wherever resources are a barrier. For more information about what support may be available, please visit OA funding and support, or email OAfundingpolicy@springernature.com or the Editor-in-Chief.
Publishing Model: Open Access
Deadline: Jul 30, 2026






Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in