How to choose autologous vs. allogeneic HCT for relapsed/refractory T-cell lymphoma?
Published in Cancer
Background
Mature T-cell lymphoma (TCL) is a heterogeneous subgroup of non-Hodgkin lymphoma (NHL) with a relatively poor prognosis compared with B-cell NHL. Among them, peripheral T-cell lymphoma, not otherwise specified (PTCL-NOS), and angioimmunoblastic T-cell lymphoma (AITL) are the two most common histological subtypes of nodal TCL in both Asian and Western countries.
Patients with relapsed or refractory (R/R) disease have a very poor prognosis. However, autologous hematopoietic stem cell transplantation (autoHCT) or allogeneic HCT (alloHCT) have been reported to result in improved survival outcomes in this salvage setting.
Several retrospective studies have compared the role of autoHCT and alloHCT for TCL [1–4]. Because these studies included patients with various levels of chemosensitivity in both upfront and salvage settings, the type of HCT that should be applied for patients with R/R disease remains to be elucidated.
What did we investigate?
The purpose of this nationwide retrospective study was to compare the role of autoHCT and alloHCT in R/R TCL.
We analyzed clinical data obtained from the Transplant Registry Unified Management Program (TRUMP), which is the registry database of the Japanese Society for Transplantation and Cellular Therapy (JSTCT).
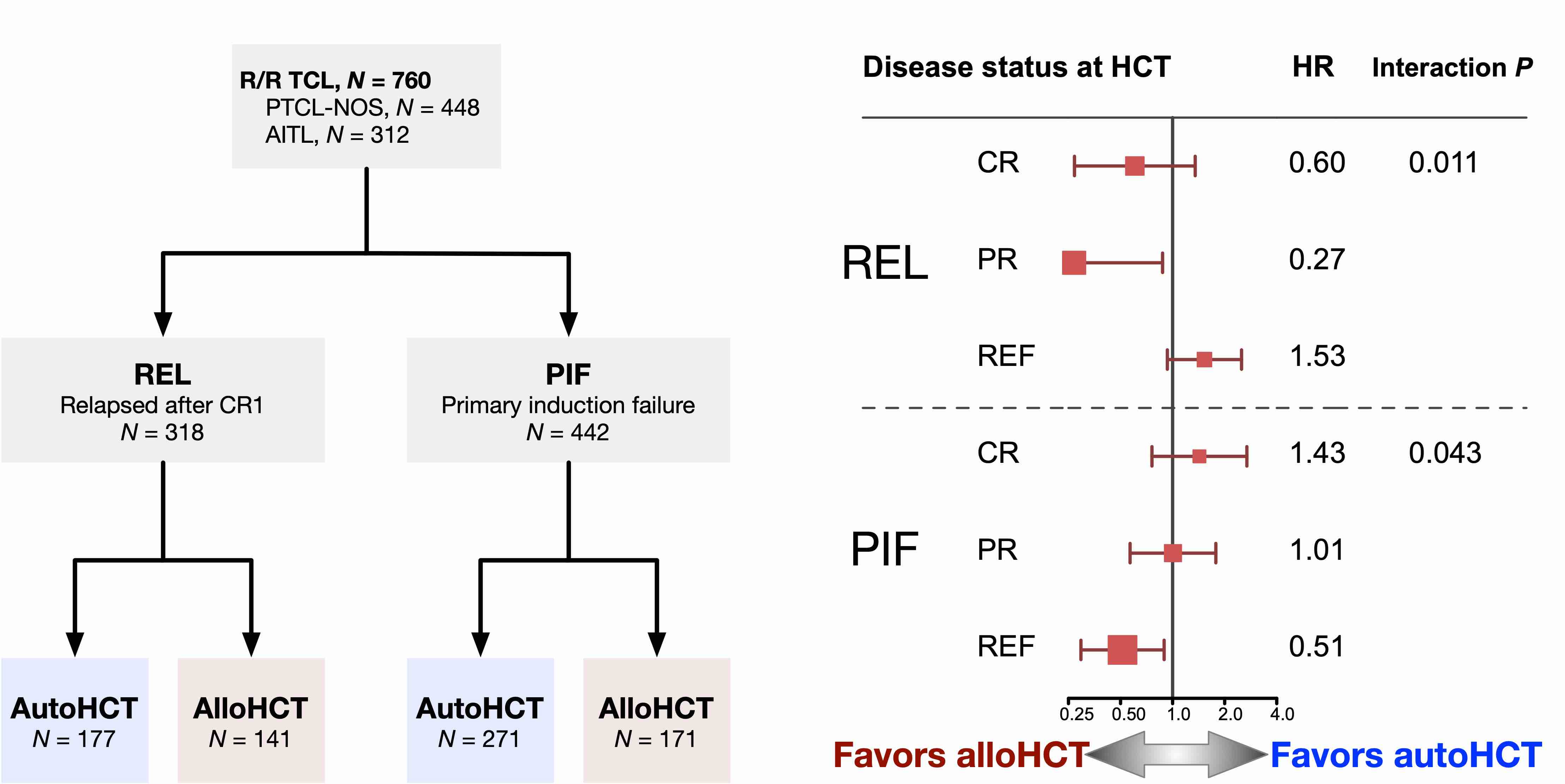
We classified patients according to their failing status of the first-line therapy, relapsed after first CR (REL), or primary induction failure (PIF), and then further categorized them by their disease status at the time of HCT as follows: complete remission (CR), partial remission (PR), and refractory (REF).
The cohort consisted of 318 REL and 442 PIF patients with PTCL-NOS or AITL undergoing their first HCT after 2–4 lines of therapy.
What did we find?
Transplant outcomes
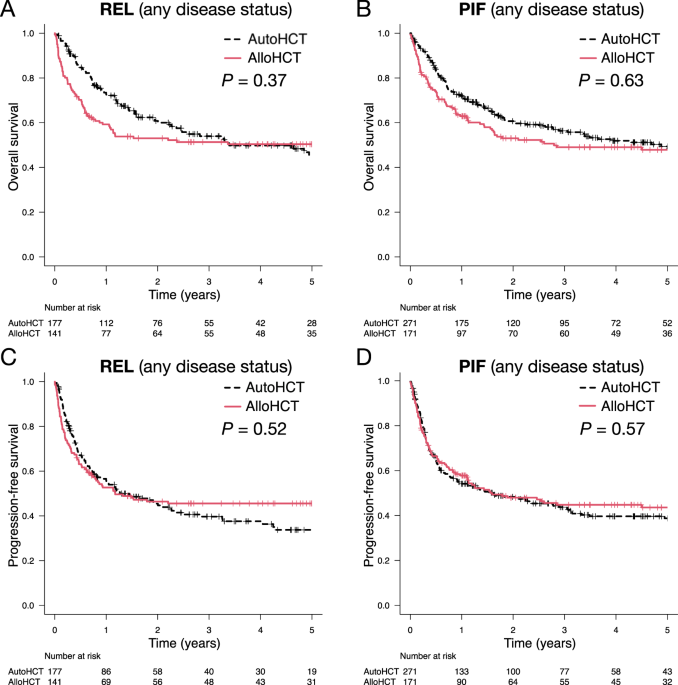
The 4-year OS of autoHCT and alloHCT recipients was 50% and 50% in the REL group, and 52% and 49% in the PIF group, respectively. The multivariable analysis showed that alloHCT had comparable outcomes with autoHCT in both the REL and PIF groups.
However, the 4-year PFS of autoHCT and alloHCT recipients was 38% and 46% in the REL group, and 40% and 45% in the PIF group, respectively. The multivariable analysis showed that alloHCT tended to be associated with better PFS in the REL group (HR 0.74; 95% CI: 0.53–1.03; P = 0.078) and was significantly associated with better PFS in the PIF group (HR 0.64; 95% CI: 0.46–0.88; P = 0.006).
Comparing alloHCT with autoHCT based on patients’ characteristics
The impact of patients’ baseline characteristics on OS comparing the two HCT types in both the REL and PIF groups were analyzed.
In the REL group, CR or PR at HCT tended to have a better OS with alloHCT, while REF did not. In addition, patient age had a moderate interaction with the HCT type (P = 0.069). This indicated that younger patients tended to have a better OS with alloHCT (HR 0.73), while older patients did not (HR 1.38).
In the PIF group, as the disease status at HCT worsens, the OS of PIF patients tends to improve with alloHCT.
Propensity-score matching analysis
Several factors had significantly different prevalence between the autoHCT and alloHCT groups. To confirm the results of the multivariable Cox model, we also performed a propensity-score matching (PSM) analysis based on the conditional probability of alloHCT assignment in both the REL and PIF groups.
In the PSM cohorts, OS of alloHCT was inferior to that of autoHCT early after HCT but became superior within 2 years after HCT and reached a plateau 3–4 years after HCT in both the REL and PIF groups. At 4 years, OS of autoHCT and alloHCT were 48% and 60% for the REL group, and 41% and 57% for the PIF group, respectively.
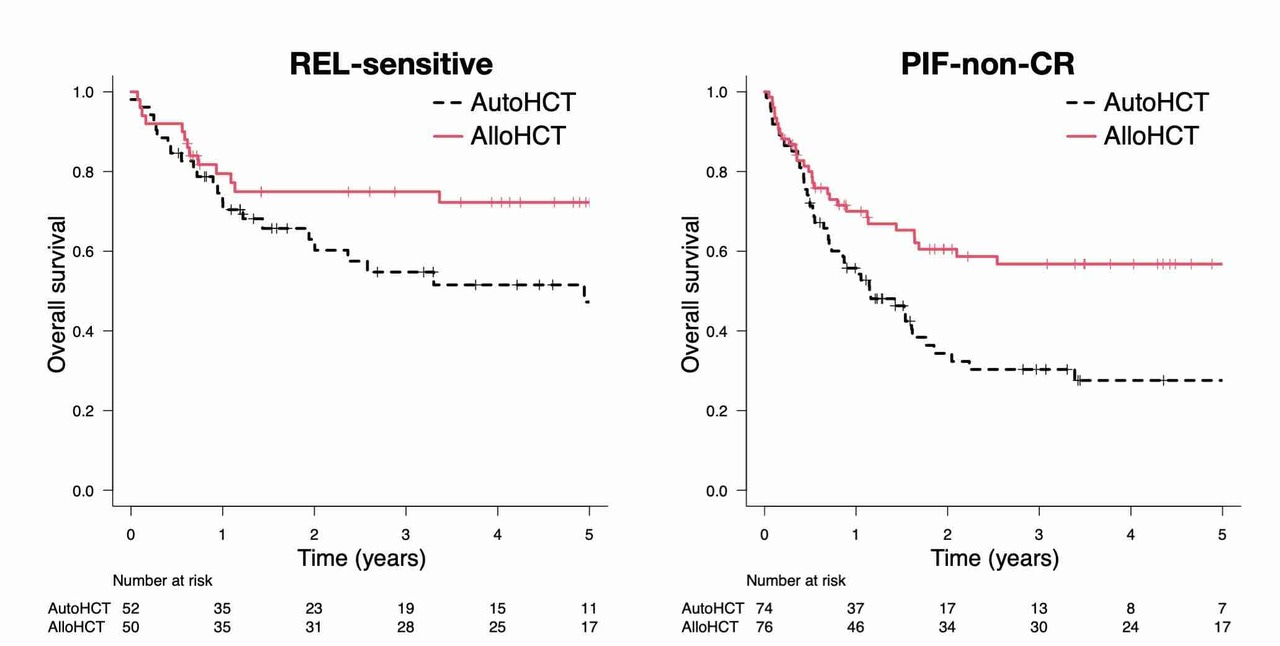
OS stratified by disease status was also analyzed in the PSM cohort. AlloHCT was associated with significantly better OS in REL-CR or -PR (REL-sensitive) disease (HR 0.50; 95% CI: 0.25–0.98; P = 0.044) and PIF-PR or -REF (PIF-non-CR) disease (HR 0.52; 95% CI: 0.33–0.83; P = 0.006) compared with autoHCT.
In terms of the histology, REL-sensitive AITL patients especially showed better OS with alloHCT (4-year OS, 80%; 95% CI, 55%–92%) compared with autoHCT (4-year OS, 47%; 95% CI, 25%–66%) (log-rank P = 0.043).
Suggestions for the treatment strategy and future clinical trials
The type of HCT had a differing impact on outcome, depending on the patient’s background. HCT type should be determined based on the response to first-line therapy and the disease status at HCT.
Additionally, patient age and AITL histology are other factors to consider. Notably, patients with REL-sensitive disease or PIF-non-CR disease can be good candidates for alloHCT if suitable donors are available.
The role of drugs with novel mechanisms of action, such as brentuximab vedotin, pralatrexate, and romidepsin, etc. in the context of HCT should be evaluated in the future.
A future study that reflects the recent progress in GVHD prophylaxis and supportive care is also warranted.
References
- Smith SM, Burns LJ, Inwards DJ, Van Besien K, Wiernik PH, Cairo MS et al. Hematopoietic cell transplantation for systemic mature T-cell non-Hodgkin lymphoma. J Clin Oncol. 2013; 31:3100–3109.
- Kim SW, Yoon SS, Suzuki R, Matsuno Y, Yi HG, Yoshida T et al. Comparison of outcomes between autologous and allogeneic hematopoietic stem cell transplantation for peripheral T-cell lymphomas with central review of pathology. Leukemia. 2013; 27:1394–1397.
- Beitinjaneh A, Saliba RM, Medeiros LJ, Turturro F, Rondon G, Korbling M et al. Comparison of survival in patients with T cell lymphoma after autologous and allogeneic stem cell transplantation as a frontline strategy or in relapsed disease. Biol Blood Marrow Transplant. 2015; 21:855–9.
- Huang H, Jiang Y, Wang Q, Guo L, Jin Z, Fu Z et al. Outcome of allogeneic and autologous hematopoietic cell transplantation for high-risk peripheral T cell lymphomas: A retrospective analysis from a chinese center. Biol Blood Marrow Transplant. 2017; 23:1393–1397.
Follow the Topic
-
Leukemia

This journal publishes high quality, peer reviewed research that covers all aspects of the research and treatment of leukemia and allied diseases. Topics of interest include oncogenes, growth factors, stem cells, leukemia genomics, cell cycle, signal transduction and molecular targets for therapy.




Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in