Managing multiple myeloma in the modern era: getting the balance right for patients
Published in Cancer
It is a very encouraging time to be a clinician treating patients with multiple myeloma (MM). We have more treatment options than ever before, with a growing number of new agents. The modern era is a far cry from 20–30 years ago, when options were limited, and patients were expected to survive for only ~3 years from diagnosis. Today, survival has doubled, and for many patients we can anticipate managing their disease for a decade or more.
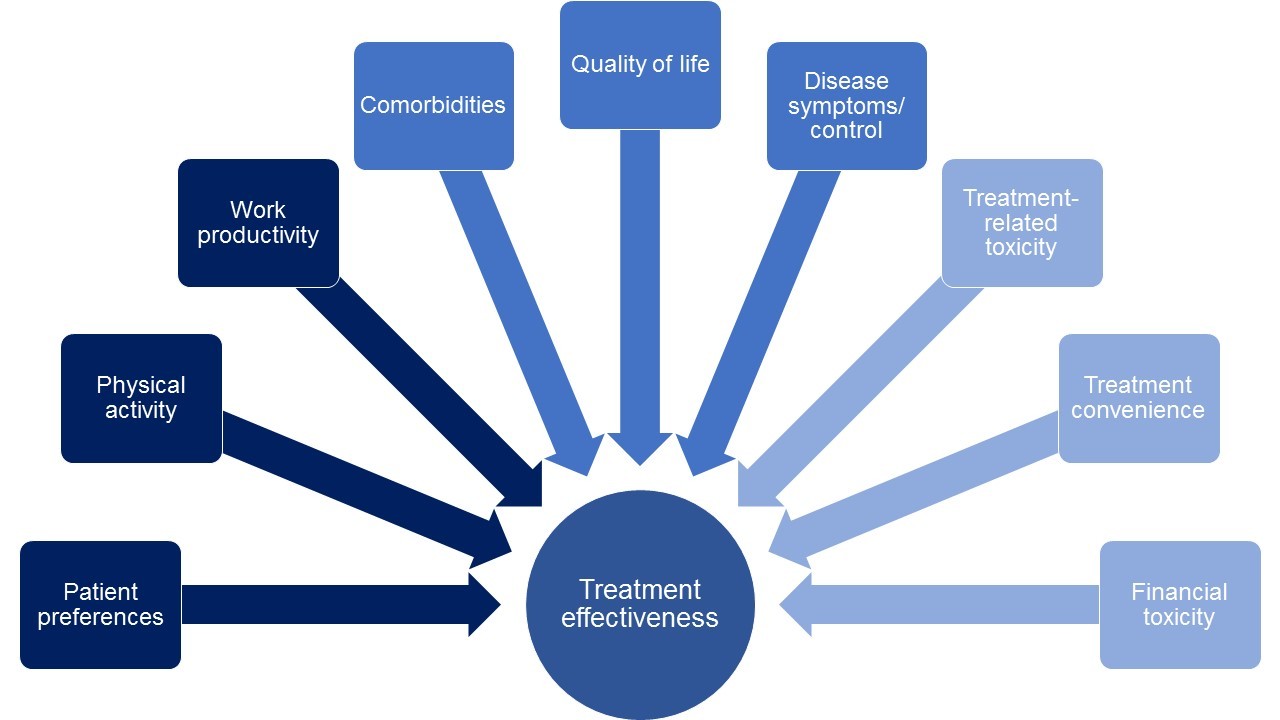
This era of novel therapies has not only extended patients’ lives but also ushered in an increasingly complex disease-management paradigm. MM is a heterogenous disease, with a diverse set of patients: some are relatively young and/or fit, and can tolerate more intensive therapy, while others are elderly and frail and require less aggressive approaches; some have rapidly progressing disease while others have more indolent disease. Because of the multitude of effective treatment options available, prescribers can now take a holistic approach to treatment. We must consider not only the effectiveness of a therapy but also its impact on patients’ quality of life.
Importantly, in addition, given the range of active treatment options, we must fully consider patients’ goals and preferences, and increasingly involve them in treatment decision-making. This consideration was a prime driver for us to write our review in Blood Cancer Journal, in which we emphasize the need to strike the right balance between conventional measures, i.e. efficacy and safety, and patient-reported measures, such as quality of life and treatment satisfaction, when making treatment choices. Many MM therapies are administered long-term; however, our patients need to be satisfied with their therapy, otherwise they will not wish to continue receiving it – consequently, effectiveness will be compromised compared to the efficacy seen with lengthy treatment duration in the more motivating circumstances of clinical trial participation.
This difference between the ‘real-world’ setting and clinical trials is another key issue. Real-world MM patients are substantially different from typical clinical trial populations, with many not being eligible for clinical trials. Consequently, when we use a treatment in routine clinical practice, the efficacy and safety data from gold-standard randomized clinical trials may not be representative of how the regimen will actually perform due to patients having more comorbidities, toxicity, treatment adherence issues, and logistical challenges related to frequent clinic visits for intravenous or subcutaneous administration of agents. These can all impact patients’ lifestyles and the feasibility of long-term treatment, along with the financial toxicity associated with treatment, and we must factor in these additional considerations when selecting a therapy.
Our review provides an overview of such additional considerations and factors that are important to patients, including symptom burden, treatment side-effects, the impact of treatment on daily activities, the costs associated with receiving treatment, and treatment convenience. We highlight how such perspectives can differ between patients – as well as over time in the same patient – and summarize ways in which patients’ perspectives can be measured. By analyzing and quantifying drivers of patients’ treatment preferences, we believe that real-world treatment decision-making and personalization of therapy will be further improved, to the benefit of all our patients.
Follow the Topic
-
Blood Cancer Journal

This journal seeks to publish articles of the highest quality related to hematologic malignancies and related disorders.

Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in