Maternal Health, Neonatology and Perinatology: Supporting Good Health and Wellbeing
Published in Public Health, Paediatrics, Reproductive Medicine & Geriatrics, and Behavioural Sciences & Psychology

Maternal health is a critical component of Sustainable Development Goal 3 (SDG3), which aims to ensure healthy lives and promote well-being at all ages. Specifically, target 3.1 aims to reduce the global maternal mortality ratio to less than 70 per 100,000 live births. Improving maternal health directly impacts neonatal outcomes as healthy mothers are more likely to have healthy pregnancies and childbirths, reducing the risks of complications and mortality for both. Addressing factors such as access to quality healthcare, skilled birth attendance, and nutrition is essential to achieving these targets and ensuring that both mothers and newborns survive and thrive. Notable strides have been made towards achieving these targets but more work must be done to improve maternal and child health outcomes.
 Maternal Health, Neonatology and Perinatology aims to publish and promote research addressing the SDG3 targets and prompt further study into improving maternal and neonatal health. Below is a summary of our top SDG3-related content on improving maternal health.
Maternal Health, Neonatology and Perinatology aims to publish and promote research addressing the SDG3 targets and prompt further study into improving maternal and neonatal health. Below is a summary of our top SDG3-related content on improving maternal health.
Maternal Mental Health
Mental health is crucial for pregnant and postpartum women because it significantly influences the well-being of both mother and baby. Pregnancy and the postpartum period are times of significant physical, emotional, and psychological changes, which can lead to stress, anxiety, and depression if not properly managed. Poor mental health during these stages can negatively affect prenatal care and maternal nutrition, potentially leading to adverse pregnancy outcomes such as preterm birth or low birth weight. Postpartum mental health issues, such as postpartum depression, can also impair a mother's ability to bond with and care for her newborn, impacting the child's long-term development. Supporting mental health during this period is vital for ensuring the health and well-being of both mother and child.
In Shiga et al, 2024 the risk factors for postpartum depression in Japan were evaluated. They performed a retrospective observational study at a single hospital, where they conducted the Edinburgh Postnatal Depression Scale (EPDS) test on 1625 women who had given birth between 2008 and 2016. The team then examined maternal, birth, neonatal and social factors, as well as breastfeeding status, to determine which factors contributed to a high EPDS score.
The results showed that maternal mental disorders and neonatal transport were significantly associated with high EPDS scores. Conversely, exclusive breastfeeding was significantly associated with low EPDS scores. The team suggests that early intervention in women at high risk of postpartum depression could prevent serious consequences such as abuse and suicide.
In addition, the transition to motherhood can be a challenging time for many women and is often characterised by high levels of stress and anxiety, which can have serious consequences if left untreated. However, informal social support provided by specially trained mentors may help to protect against postpartum depressive symptoms.
In a recent study (Gasperowicz & Benzies, 2024), researchers evaluated the association between different types of mentors and women’s depressive symptoms during the transition from pregnancy to postpartum. The team used data from a community sample of 312 first-time mothers who participated in the Welcome to Parenthood program. The program provided education and mentorship for women during this transition period.
They found that women who were mentored by their mothers or sisters scored the lowest on the EPDS. Those mentored by their mothers-in-law scored the highest. However, women who were mentored by other family members, friends or volunteers scored between these two extremes. These results suggest that support provided by mothers or sisters is best for women’s mental health and the study highlights the importance of tailored support systems for new mothers, especially those who have recently relocated and lack traditional family support.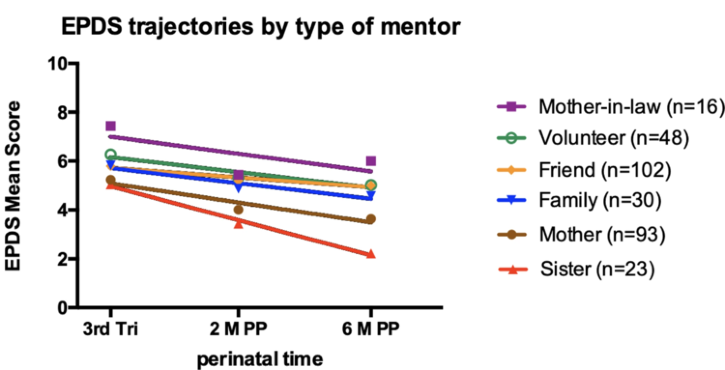
Maternal Healthcare
Prenatal and antenatal care play a crucial role in ensuring a healthy pregnancy and safe childbirth. These regular medical check-ups allow healthcare providers to monitor the progress of the pregnancy, identify and manage potential risks or complications early, and provide essential education on nutrition, exercise, and childbirth preparation. Adequate prenatal care helps detect conditions like gestational diabetes, preeclampsia, or fetal growth issues, which can be addressed promptly to prevent serious outcomes. Additionally, antenatal care supports the mental and emotional well-being of the mother by offering guidance and reassurance throughout her pregnancy. By ensuring that both the mother and baby are healthy and well-prepared for birth, prenatal and antenatal care are fundamental to reducing maternal and infant mortality rates and promoting long-term health.
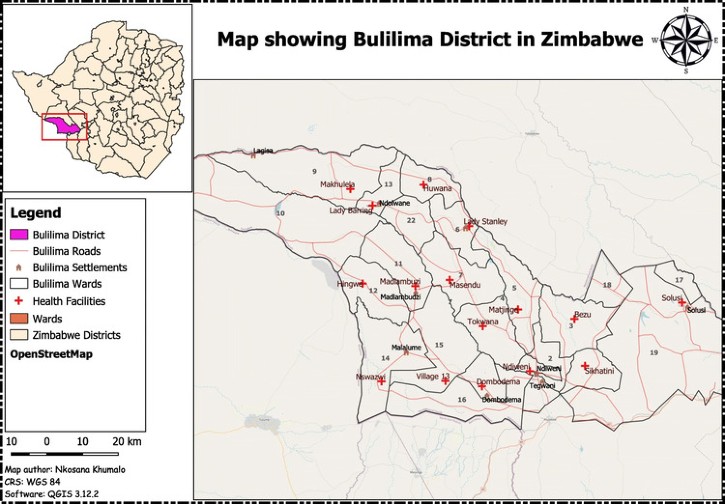
In Zimbabwe, traditional medicine is often used to treat a variety of health conditions. However, the relationship between traditional medicine and maternal health outcomes is not well understood. Mudonhi & Nunu, 2021 investigated the relationship between traditional medicine use and maternal complications during antenatal care. The team conducted a survey with 185 women who were randomly selected to participate. The women were asked about their use of traditional medicine and self reported any complications during pregnancy. The results showed that 29% of the women had experienced complications though the proportion of women who developed complications was higher in those that did not use traditional medicine compared to those that did (30% and 26% respectively).
The findings suggest that there is a significant relationship between the use of traditional medicines and a reduced risk of experiencing maternal complications. Further research is needed to understand the active ingredients in these medicines and how they may be integrated into modern health systems to improve maternal health outcomes.
Maternal healthcare is essential for safeguarding the health and well-being of mothers and their children, both during and after pregnancy. By ensuring access to quality prenatal, antenatal, and postnatal care, we can significantly reduce the risks of complications, improve health outcomes, and support the mental and physical health of mothers and their babies. Maternal Health, Neonatology and Perinatology is committed to advancing research in this critical field, providing valuable insights and evidence to improve maternal healthcare practices worldwide. Together, we can work towards a future where every mother and child receives the care they deserve.
Follow the Topic
-
Maternal Health, Neonatology and Perinatology

This is an open access, peer-reviewed journal that considers articles on topics related to the physiological and pathological conditions of women during preconceptional, perinatal, and postpartum periods; and of fetuses and newborn infants during and beyond their initial hospital stay.
Related Collections
With Collections, you can get published faster and increase your visibility.
Novel interventions to improve the survival in extremely low gestational age neonates (ELGANs)
This topic, which is at the core of every neonatologist’s heart, is meant to promote the recent advances, interventions, and protocols that can help us improve the overall outcome of intact survival in neonates who are less than 28 weeks gestational age at birth. These neonates require specialized care and the management strategies for older neonates may not apply to them. This issue aims to showcase these variations from usual neonatal care for ELGANs.
There shall be a special focus on the management strategies and scalable models for the management of such neonates in low-resource settings. A critical examination of existing practices for the care of ELGANs in the myriad of neonatal intensive care units across the world will be done, and the necessary reforms will be delved into. The role of artificial intelligence in the management of such neonates shall also be explored.
Neonatal mortality contributes to a major portion of under-five mortality and prematurity is a leading cause for the same. This issue shall not only focus on the postnatal treatment strategies for ELGANs but also on the antenatal preventive strategies to prevent prematurity overall and to allow a neurologically intact survival if the neonate is born prematurely.
By amalgamating these various strategies and time points of interventions, this issue aims to showcase a detailed overview of the current practices, advancements, and possible fields for future research in the management of this vulnerable subgroup of neonates.
This Collection supports and amplifies research related to SDG 3, Good Health and Well-Being.
We are committed to supporting participation in this issue wherever resources are a barrier. For more information about what support may be available, please visit OA funding and support, or email OAfundingpolicy@springernature.com or contact the Editor-in-Chief.
Publishing Model: Open Access
Deadline: Mar 10, 2026
Integrated Perinatal and Postnatal Strategies for Infants with Prenatal Substance Exposure
As the prevalence of opioid and polysubstance use during pregnancy continues to rise globally, there is an urgent need to reframe how we support both mothers and infants affected by in utero substance exposure. This issue will spotlight innovative, multidisciplinary care models designed to optimize outcomes for neonates at risk for or diagnosed with Neonatal Abstinence Syndrome (NAS).
A special focus will be placed on integrated care approaches that span the perinatal continuum—from antenatal counseling and addiction support to postnatal management of NAS. Co-located and collaborative services involving obstetricians, addiction medicine specialists, neonatologists, mental health providers, and social workers will be highlighted for their impact on maternal engagement, breastfeeding success, and reduction in NICU length of stay. Models such as "rooming-in" and the Eat, Sleep, Console (ESC) method will be critically examined for their scalability and applicability to the population.
This issue will also explore the long-term growth and neurodevelopmental outcomes infants with prenatal substance exposure, emphasizing the confounding influence of poverty, caregiver instability, and trauma. Attention will be given to the role of early intervention services, predictors of resilience, and the pressing need for standardized follow-up protocols to support optimal cognitive, behavioral, and motor development.
By bringing together clinical innovations, public health perspectives, and developmental follow-up strategies, this issue aims to foster a comprehensive understanding of how to promote long-term well-being including optimal growth and neurodevelopmental outcomes for in this uniquely vulnerable population.
This Collection supports and amplifies research related to SDG 3, Good Health and Well-Being.
We are committed to supporting participation in this issue wherever resources are a barrier. For more information about what support may be available, please visit OA funding and support, or email OAfundingpolicy@springernature.com or contact the Editor-in-Chief.
Publishing Model: Open Access
Deadline: Mar 12, 2026





Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in