Nutrition knowledge, dietary diversity, and household food security among mothers of under-five children in Abakaliki, Ebonyi State, Nigeria.
Published in Public Health
Public health nutrition research often begins with statistics. For me, this study began with people—specifically, mothers and children I met during my internship as a Nutrition Officer at the Nutrition Department of the Ministry of Health in Ebonyi State, Nigeria.
During this period, the department was collaborating with Helen Keller International to implement a programme called Transforming Lives Through Nutrition. One of the core components involved the administration of Ready-to-Use Therapeutic Food (RUTF) for children under five suffering from severe acute malnutrition. Day after day, I witnessed the remarkable short-term recovery these children made once they were enrolled in the programme.
But alongside this progress came an unsettling question that would eventually give birth to this research.
I found myself asking: What happens to these mothers and children if the programme folds up tomorrow? Because USAID programme at the time, conversations were already emerging about funding uncertainties. What if Transforming Lives Through Nutrition also disappears, what safety net remains? More importantly, do mothers have the practical means—not just the knowledge—to sustain good nutrition using locally available foods?
These questions stayed with me and became the foundation of our study: Nutrition knowledge, dietary diversity, and household food security among mothers of under-five children in Abakaliki, Ebonyi State, Nigeria.
From Observation to Research Question
Nutrition advocacy has made significant strides in Nigeria. Mothers are increasingly exposed to messages about exclusive breastfeeding, complementary feeding, and child care through health facilities and community campaigns. Indeed, much of the published literature focuses on what mothers know.
However, during my field experience, a troubling pattern was evident. Many mothers could correctly describe recommended feeding practices, yet still presented with malnourished children. This contradiction forced us to rethink a central assumption in nutrition programming: knowledge automatically leads to action.
Our study was designed not to dismiss nutrition education, but to interrogate its limits.
What We Found: A Knowledge–Implementation Gap
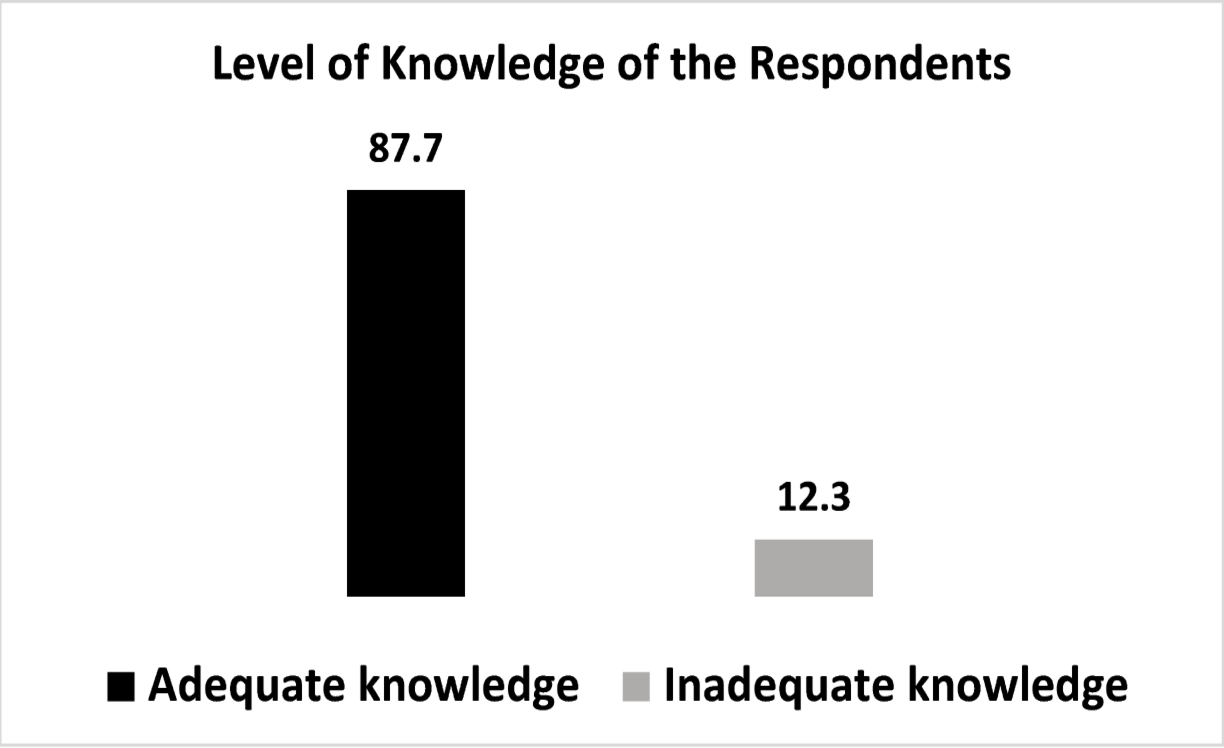
The findings were striking. An overwhelming majority of mothers demonstrated adequate nutrition knowledge. They understood exclusive breastfeeding, the importance of continued feeding during illness, and the basics of child nutrition. On paper, this looked like success.
Yet beneath this encouraging surface lay a harsher reality.
More than two-thirds of households were severely food insecure. Dietary diversity among women was suboptimal, with limited consumption of nutrient-dense foods such as eggs, dark green leafy vegetables, and dairy products. In practical terms, mothers knew what their children should eat—but often could not afford it, access it, or prioritize it within complex household dynamics.
This exposed a critical truth: knowledge without the means to implement it produces the same outcome as no knowledge at all—continued child malnutrition.
Why Implementation Fails
Our interactions with mothers revealed that poor implementation was not due to negligence or indifference. Instead, it was shaped by structural and social constraints:
Poverty and food access: Many households relied on monotonous staple diets, not by choice but by necessity.
Household decision-making: Mothers often lacked autonomy over food purchases and distribution.
Cultural practices: Persistent beliefs around herbal remedies and breastfeeding during pregnancy continued to influence behaviour.
Programme dependency: Emergency nutrition interventions saved lives but were not always paired with sustainable, food-based solutions.
In essence, mothers were being asked to practice “ideal nutrition” in non-ideal circumstances.
Why This Matters for Public Health
This research reinforces an uncomfortable but necessary message for public health nutrition: information alone does not change outcomes in contexts of deprivation.
Nutrition education remains vital, but it must be embedded within broader systems that address food security, livelihoods, gender dynamics, and access to diverse local foods. Without this, we risk placing responsibility on mothers for outcomes largely determined by structural conditions beyond their control.
Our findings align with global nutrition priorities, including the Sustainable Development Goal 2 (Zero Hunger), which emphasizes not only knowledge, but access, availability, and utilization of nutritious food.
Looking Forward: Rethinking Future Interventions
Future research and programming must shift focus from whether mothers know to why mothers cannot act on what they know. This includes:
Investigating barriers to translating knowledge into practice
Integrating nutrition education with food-based livelihood support
Promoting locally available, affordable dietary solutions
Designing culturally sensitive, community-led behaviour change strategies
Evaluating sustainability beyond donor-funded interventions
Only by addressing these dimensions together can nutrition knowledge become truly transformative.
A Personal Reflection
This study is deeply personal to me. It represents a transition from observing problems in the field to systematically documenting them, with the hope of influencing policy and practice. The mothers I met were not lacking in awareness—they were navigating constraints with resilience and dignity.
If this work contributes even modestly to reframing how we design nutrition interventions—away from knowledge alone and toward implementation-focused solutions—then it has achieved its purpose.
Because in public health nutrition, the real measure of success is not what people know, but what they are realistically able to do.
https://doi.org/10.1186/s12982-025-01310-1
Follow the Topic
-
Discover Public Health

This is an open access journal publishing research from all fields relevant to public health.
Related Collections
With Collections, you can get published faster and increase your visibility.
Antimicrobial Resistance: The New Challenge to Global Health in a Post-Pandemic World
Antimicrobial resistance (AMR) is a seriously ongoing threat to global health, occurring when bacteria, fungi, viruses, and parasites evolve to resist the drugs designed to kill or block them. The COVID-19 pandemic has both directly and indirectly exacerbated the problem of AMR, as the overuse of antibiotics has accelerated the development of resistance in many pathogens. COVID-19 may have subsided, but AMR continues to pose a significant risk to the effectiveness of global healthcare systems, threatening to reverse decades of progress in combating infectious diseases. The interplay between population health and AMR has become increasingly critical as healthcare practices have shifted in response to the pandemic. Understanding this relationship is essential for developing effective strategies to mitigate the impact of AMR on population health in a post-COVID context.
The motivation for launching this Collection arises from the urgent need to address the rising tide of AMR as healthcare systems grapple with the long-term effects of the pandemic. Increased antibiotic use during COVID-19 treatment, changes in healthcare access, and disruptions in public health interventions have all contributed to an environment where AMR can thrive. Moreover, the pandemic has highlighted the importance of a multidisciplinary approach to tackling AMR, involving epidemiology, policymaking, and community health initiatives. This Collection aims to provide a platform for researchers and practitioners to share insights and findings that can inform future strategies to combat AMR while considering the broader implications for population health.
This Collection aims to highlight the multifaceted nature of AMR in a post-pandemic environment. We solicit articles that investigate the particular issues provided by the pandemic in terms of AMR development and containment, examine the impact of AMR on many sectors of healthcare, and propose novel strategies to minimize resistance propagation. Submissions may include original research, policy assessments, program evaluations, and comments on the following major areas:
• Epidemiology and trends of AMR post-pandemic
• Impact of COVID-19 on antibiotic usage
• Surveillance strategies for AMR
• AMR and stewardship
• Prevention and control measures to limit AMR spread
• Policies and programs to promote antibiotic stewardship
• Economic and social implications of AMR
• Global collaboration and initiatives to tackle AMR
By addressing these critical issues, this Collection aims to provide a comprehensive understanding of the emerging challenges in antimicrobial resistance in a post-pandemic world and to promote effective strategies to preserve the power of our current antimicrobials.
Keywords: antimicrobial resistance; COVID-19; antibiotics; global health; infectious diseases; public health; policy; prevention
This Collection supports and amplifies research related to SDG 3.
Publishing Model: Open Access
Deadline: Jun 30, 2026
Health Literacy and Informal Caregiving
Personal and health service literacy limitations are significant predictors of poor healthcare access, suboptimal health behaviors (e.g., physical inactivity, smoking), and adverse outcomes, leading to increased emergency visits, hospitalizations, and premature mortality—particularly among informal caregivers and their care recipients. Informal caregivers, especially in low- and middle-income countries (LMICs), often make critical health and healthcare decisions that impact both their own outcomes and those of the individuals they care for. Therefore, interventions aimed at enhancing health literacy among informal caregivers are essential for improving health outcomes, healthcare utilization, and lifestyles. We invite submissions addressing, but not limited to, the following topics:
We invite submissions addressing, but not limited to:
1. Health literacy assessments of informal caregivers
2. Sociocultural determinants of caregiver health literacy
3. The impact of health literacy on caregiver burden, health status, and outcomes
4. Interventions to promote health literacy among informal caregivers
Submissions from low- and middle-income countries are highly encouraged, while studies from high-income countries will also be considered based on their novelty, robustness, and strength of evidence.
This Collection supports and amplifies research related to SDG3 and SDG10.
Keywords: Health literacy; informal caregiving; wellbeing; quality of life; health equity
Publishing Model: Open Access
Deadline: Feb 28, 2026


Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in