Our complex universe within: Merging mental and brain health
Published in Social Sciences

Imagine a curious alien landing on Earth in search of knowledge. While observing humans, the extraterrestrial is puzzled by the dichotomy between psychiatry (mental health) and neurology (brain health). "Why," it wonders, "do they view these as separate phenomena? They seem so intimately intertwined and similar!" Somewhat humorously, the alien considers starting a cosmic podcast titled Minds, brains, and other human misunderstandings.
This alien's confusion mirrors our struggle to understand the intersection of mental and brain health. The historical divide between psychiatry and neurology primarily shapes our conceptualization of these domains. However, recent evidence challenges these constraints, revealing an entangled nature of mental and brain health. This knowledge can lead to more effective prevention and intervention strategies, which was the primary motivation for our paper published in Nature Mental Health.
Health and disease spectra
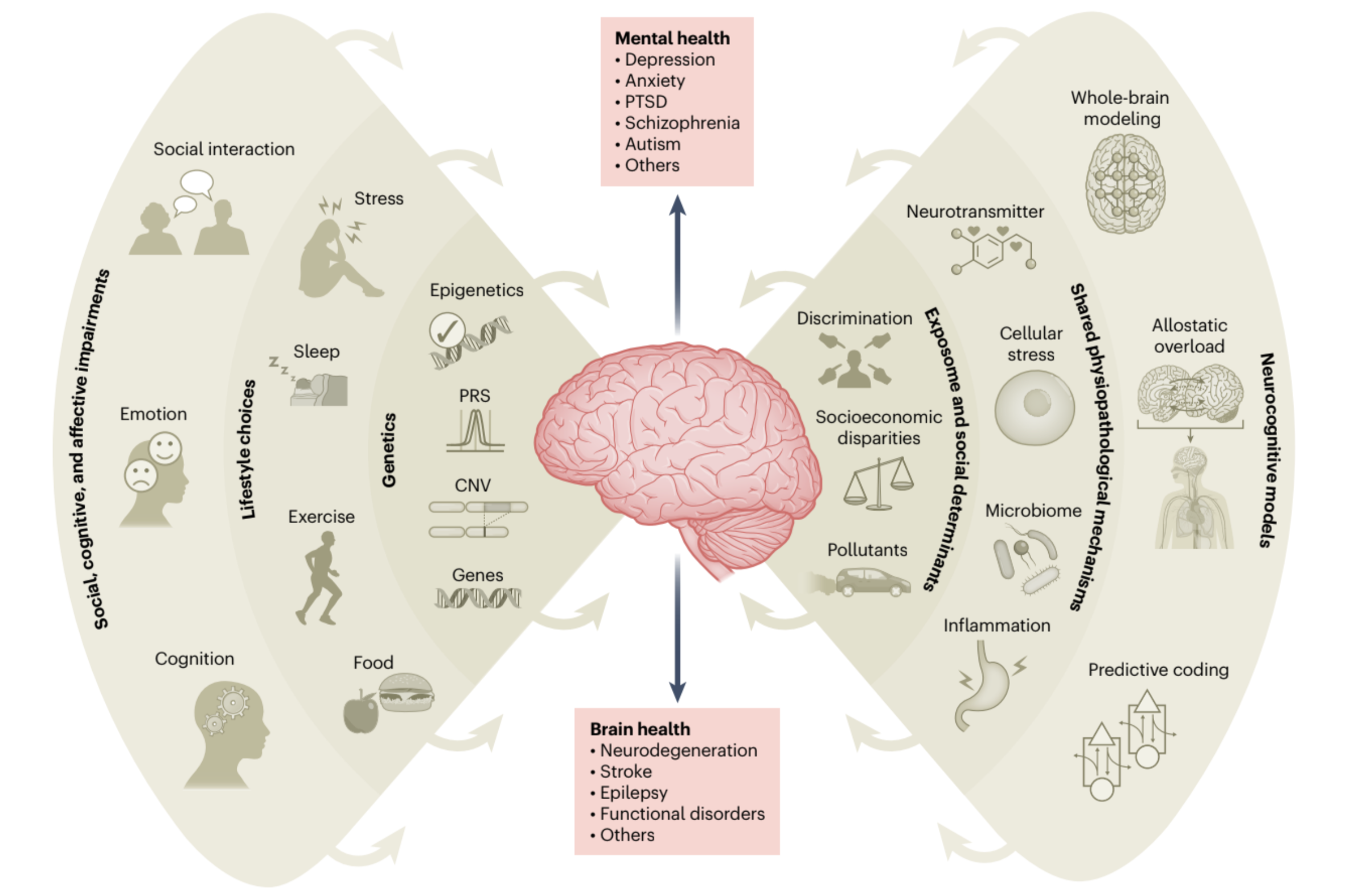
Evidence suggests that the etiology of psychiatric and neurodegenerative disorders, typically treated separately, shares many commonalities. They have partially shared origins in neurodevelopment and are influenced by an array of interconnected elements: genes and epigenetics, environmental pollutants, social determinants, cumulative effects of lifestyle choices across the lifespan, and shared neurocognitive and pathophysiological features (see Figure).
From genes to the exposome
Specific genes can increase the risk for psychiatric and neurological diseases, as can structural variations in our genome (i.e., copy number variations - CNVs) or polygenic risk scores. Epigenetic changes can be influenced by our social and environmental conditions and, in turn, impact both psychiatric and neurological disorders. Poor nutrition, pollutant exposure, socioeconomic status, and social isolation can affect mental and brain health. Physical inactivity, sleep disturbances, substance abuse, stress, and obesity also contribute to psychiatric and neurological outcomes.
Mechanistic explanations and computational modeling
Psychiatric and neurological disorders share multiple pathophysiological pathways, just as shared motifs and themes often underpin complex narratives. Inflammation and neurotransmitter changes caused by unhealthy lifestyle choices can impact diseases ranging from stroke to depression. The same applies to cellular stress, microbiome, and metabolic processes.
Integrative models provide a more dimensional approach to different psychiatric and neurological diseases. Predictive coding theories align brain predictions, interoceptive signal, and sensory data. Allostatic overload refers to multilevel processes responding to persistent environmental demands, affecting health across the body and brain. Computational synergetics unite experimental data and computational models to analyze brain interactions, providing a more holistic view of different mechanistic processes in disease. These models integrate external factors, omic influences, and neuroimaging findings and are applied to various conditions for comprehensive mechanistic insights. Crucial for a dimensional mental and brain health approach, these models enable an integrated understanding of shared mechanisms and brain dynamics across psychiatric and neurological disorders.
A call to action
With a nascent but multilevel, shared understanding of mental and brain health, we can bridge the gap between psychiatry and neurology, potentially leading to groundbreaking discoveries. As we start embracing the symphony of influences on our mental and brain health, developing more transdisciplinary, holistic, integrated, and dimensional theories is necessary. Let's take a cue from our imaginary alien friend and challenge the status quo. Mental health is not essentially different from brain health, but these are two descriptive analyses of the same harmonious symphony of health.
* Figure credits (poster image): Lucas Neufeld & Agustin Ibanez
Follow the Topic
-
Nature Mental Health

This journal takes an expansive view of the relationship between mental health and human health. It brings together innovative investigation of the neurobiological and psychological factors that underpin psychiatric disorders to contemporary work examining the effects of public health crises.






Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in