Pregnancy tracking with wearables
Published in Public Health and Anatomy & Physiology
Explore the Research

Biometrics of complete human pregnancy recorded by wearable devices - npj Digital Medicine
npj Digital Medicine - Biometrics of complete human pregnancy recorded by wearable devices
President Biden stated in his 2024 State of the union that “Women are more than half of our population but research on women’s health has always been underfunded.” Perhaps even more strangely, pregnancy, which affects every single person on this planet, is rarely studied, relegated to one niche of women’s health. Historically, funding has focused on conception or labor; when discussing this project with funders, we were told “nobody could study all of pregnancy. Are you studying conception, or a specific pathology?” So, we used discretionary funds from the opening of the Smarr lab and moved ahead. Funders often must think about what has worked before. It is not easy to see how transformative personal data trails can be – continuous data generated on each individual capturing the biological dynamics in a way that the old model – one blood draw, one consult – were not able to see and so were designed to function without. Now it is possible to study all of pregnancy. Wearables, smartphone, and internet of things (IoT) broadly are enabling more of life – and more lives – to leave a record. As the social media star Farideh has put it in her recent song, ‘we never really studied the female body’. Our lab, and those individuals participating to make their lives count on the scientific record, are trying to help change that.
Biometrics of Complete Human Pregnancy Recorded by Wearable Devices
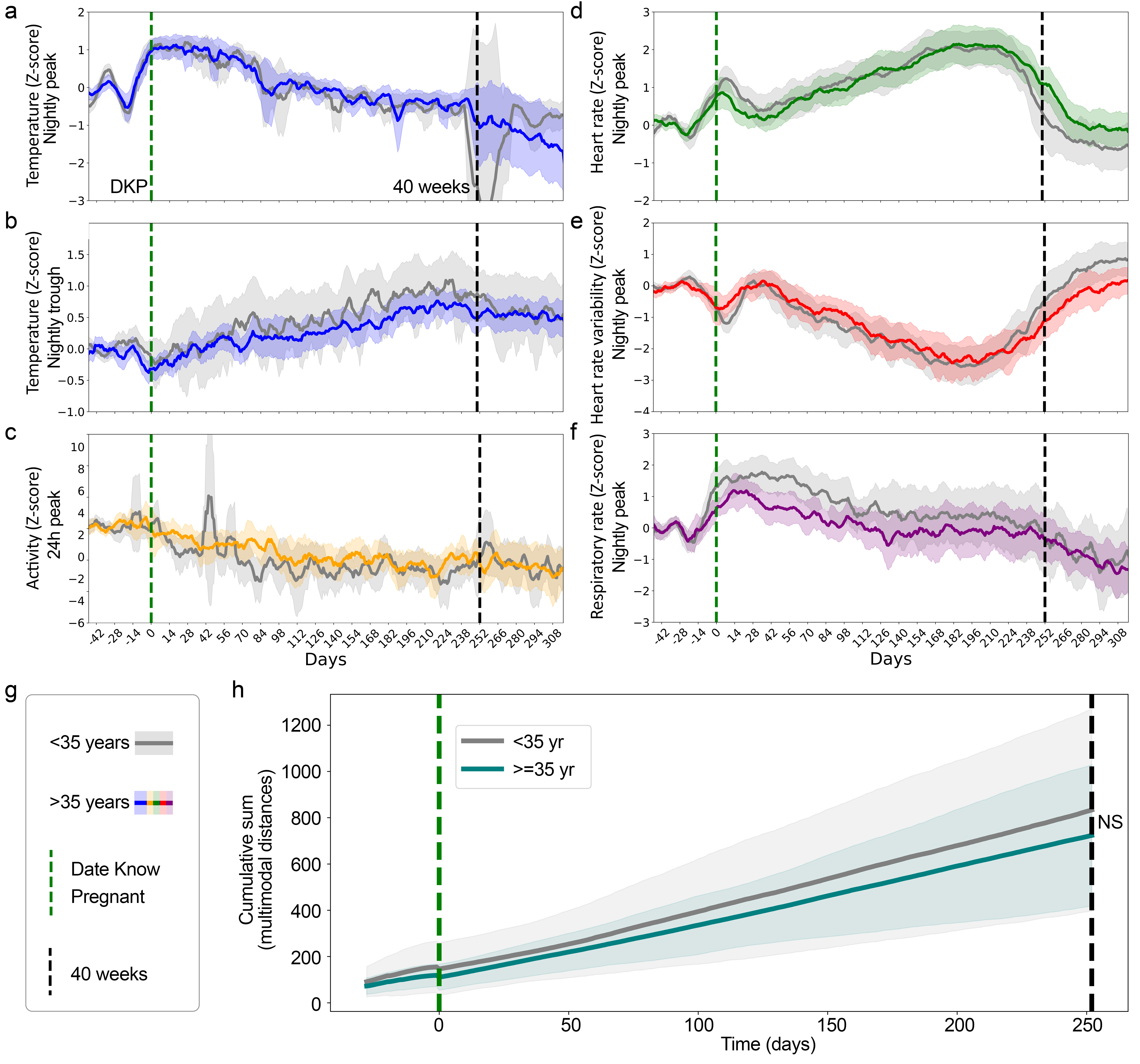
In a recent manuscript ("Biometrics of complete human pregnancy recorded by wearable devices", https://rdcu.be/dQDmK), we conducted analyses on wearable device data that was voluntarily shared with researchers from 120 individuals throughout their pregnancy. As data are continuously collected by wearable devices, the patterns revealed therein capture signs of maternal health continuously, as opposed to biometrics (e.g. temperature, heart rate) measured at prenatal appointments where patients are often experiencing heightened stress, and which might happen only once every few weeks. Single point measurements may reflect the time of day of the visit as much as changes relevant to the pregnancy.
With multiple data types, distal body temperature, heart rate, heart rate variability, respiratory rate, and activity, we found that each data type, or modality, demonstrated a different pattern as time passed. All changed across pregnancy, but in different and complementary ways, so that no one sensor type can tell the whole story. On average, each of the modalities changed throughout pregnancy relative to each individual's data prior to pregnancy onset. For example, nightly peak temperature, the hottest time in each night of sleep, was the most different during the beginning of the first trimester following conception, whereas for heart rate, the maximum deviation from a pre-pregnancy state occurs near the end of the third trimester. Additionally, when we aligned all the data by the end of pregnancy, i.e. delivery, we see that heart rate and respiratory rate decline prior to labor, while heart rate variability increased, and temperature dipped following labor.
Having maps like this allows others to start to build tools that can detect changes from these expected trajectories in order to draw attention to possible changes in health that might require a visit or a deeper look. Characteristic changes may be useful to clinicians to detect deviations from ‘normal’ that might indicate risk for complications. Also, for individuals without access to consistent prenatal care, visibility into their own wearable data during pregnancy may allow them to monitor their own health better than without this kind of visibility, especially for those with a lack of health insurance or residing in health care deserts. Medical dashboards drawing on data like this can be used to support virtual clinical visits too, which might reduce some of the burden on pregnant individuals who can not easily come to the clinic over and over due to remote location, job obligations, or long transit times.
We note that currently, there is no standards for wearable data utility in clinical care, as this type of analysis has not been possible until recently. We hope that our work will provide a step towards continuous monitoring in maternal health care, but to understand manifestations of pregnancy complications, we would need a lot of different pregnancies with different outcomes to build generalizable detectors for the many possible complications that can arise during pregnancy. As pregnancy is so understudied, it might well turn out that complications look different in different groups of people. We don’t know. In our study, individuals voluntarily shared their personal wearable data paired with personal experiences collected via a survey. This study shows that transformation of women’s health knowledge could be fueled by women choosing to share their data over time in different studies and with different communities; it will have to evolve over time, but we believe that if people see what is possible, then it will happen much faster and more equitably than waiting for traditional studies alone.
Continuous health monitoring has the potential to enhance personalized health care. The bar for improvement may be lower than it seems. For example, 35 years old is a common age threshold for labeling a pregnancy as ‘high risk’ (previously termed ‘geriatric’ pregnancies but now are more commonly labeled as pregnancies at an ‘advanced maternal age’). This label often comes with increased imaging, and genetic and other testing to identify potential pregnancy complications. The increased caution is a good idea but comes at a cost to the mother as well as the system, so if there was an additional way to refine who is really at risk, that would be helpful on all sides. We did not see a significant difference in physiological data collected from individuals who were over or under the age of 35 during pregnancy. That is, on average, both groups look about the same. This isn’t surprising – we doubt a woman’s physiology changes radically on her 35th birthday (even without a lot of studies on aging in women, we feel good about this guess). On the other hand, as women with complications or other events share the record of their physiology through those events, we (all) will be able to refine the pattern detection that can identify and eventually, hopefully, predict who really needs that extra testing and early intervention. Wearable data should be used more broadly to refine health categorizations that previously relied on large generalizations such as age. Wearable data may also allow for health insights during pregnancy that infrequent office visit measurements can detect.
A Personal Postscript: Lauryn’s Pregnancy through a wearable device
At first, lead author of the manuscript that prompted this post, graduate student Lauryn Bruce was inspired to work on wearable data in pregnancy after reading an anonymous blog post from a woman who saw trends in their wearable data that mimicked that of a past miscarriage. With no physician expert in wearables to turn to, this woman’s only resource was other women on the internet. During her research, Lauryn also became pregnant, and happened to be wearing an Apple Watch throughout her pregnancy. Now as not just a researcher, but a mother-to-be, she was ecstatic to know that she was collecting data throughout her pregnancy. Following recovery, she downloaded and parsed her own data with help from a Median blog post written by Vinayak Gaur, and set to finding trends in her own data.
In the images below, you can see her resting heart rate data throughout her pregnancy (top) and on the day before and during labor (bottom). Combining timestamps from her own memory and electronic health records, she found trends that not just reflect her experience, but also adhere to the trends found across the 97 pregnancies in her published manuscript. Lauryn said “I hope that this work will help individuals to interpret their own data, understand their physiological changes throughout pregnancy, and provide people another tool to advocate for themselves when communicating with their provider.” I hope so too, and I hope that as a society we learn how to support people interested in sharing their experiences this way. With a digital record to match, everyone’s life could be helping everyone else’s in ways that the old medical model was never designed to provide. Sure, we didn’t use to study the entirety of pregnancy at once, let alone all of life, but now we can, so maybe we should think about how to do that safely and equitably going forward.

Follow the Topic
-
npj Digital Medicine

An online open-access journal dedicated to publishing research in all aspects of digital medicine, including the clinical application and implementation of digital and mobile technologies, virtual healthcare, and novel applications of artificial intelligence and informatics.
Related Collections
With Collections, you can get published faster and increase your visibility.
Digital Health Equity and Access
Publishing Model: Open Access
Deadline: Mar 03, 2026
Evaluating the Real-World Clinical Performance of AI
Publishing Model: Open Access
Deadline: Jun 03, 2026


Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in