Reactogenicity following Vaccination via Smartwatches
Published in Healthcare & Nursing

Modern wearable devices are capable of passively and longitudinally monitoring physiological signals, such as the daily resting heart rate or temperature, and behavioral signals, such as activity and sleep. Smartwatches and activity trackers, which are now worn by one in five Americans, can improve our ability to objectively characterize each individual’s unique baseline. With this data, we can see when participants fall out of their normal range for sleep, activity level or resting heart rate; deviations from individual norms may indicate that they are coming down with a viral illness or infection.
Large platforms like the Digital Engagement & Tracking for Early Control & Treatment (DETECT) platform, now collecting data from 40,000 individuals, have been used to identify COVID-19 positive cases through a mobile app, demonstrating for the first time that wearable sensors can identify cases with greater success than looking at symptoms alone.2 Such a continuous monitoring also provides a way to track individual’s physiological and behavioral metrics:
- pre-infection: defining an individualized baseline and expected variations from baseline3
- during the infection: detecting the infection before a traditional COVID test,4 and
- post-infection: monitoring participants that may suffer from long-COVID.5
Focusing on the infection period, we developed an explainable prediction model to detect a COVID-19 infection, which adapts also to the absence of self-reported symptoms, works with any sensor data, and explains the importance of each feature.4
Beyond the infection, we have investigated also the reactogenicity post-vaccination, exploring how this is associated with factors that are linked to immunogenicity, providing a potential proxy to approximate immune-response. While the relationship between reactogenicity and immunogenicity needs to be quantified with prospective trials, our study and other recent studies have quantified the vaccine reactions,1,6 and measured a correlation with immunogenicity.7
Thanks to the 7728 individuals who shared the information of their COVID-19 vaccinations, we were able to study the physiological changes post-vaccination. Our analysis showed that the average resting heart rate of study participants increased significantly the day following vaccination, peaking two days post-vaccination, and returning to normal four days after the first dose and six days after the second. The increases in resting heart rate are higher after the second dose of the Moderna versus the Pfizer-BioNTech vaccine, as previously reported by subjective assessment of reactogenicity. Prior COVID-19 infection was linked with a significantly higher resting heart rate increase after the first vaccine dose relative to those without prior infection. (Figure) This increase is consistent with an expected greater immune response for these individuals, making resting heart rate a potential digital, objective biomarker of reactogenicity.
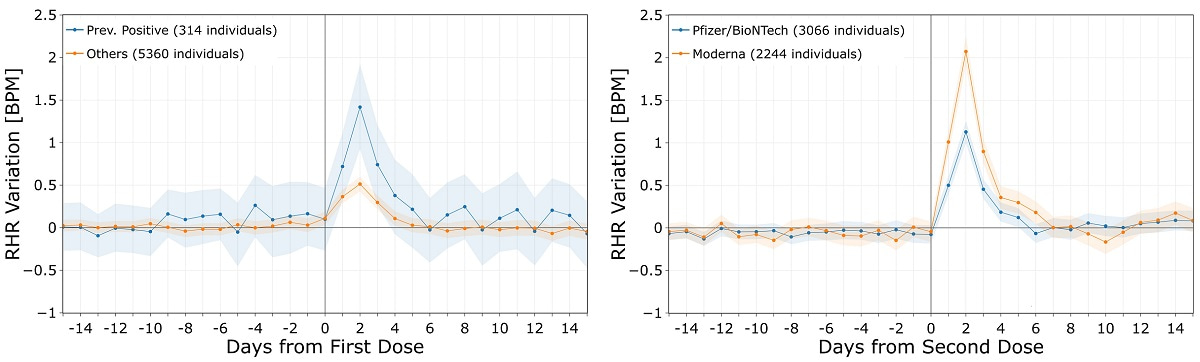
We also explored individual behavioral changes following vaccination via measured changes in a person’s routine sleep and activity. We identified significant associations between individual behavioral changes (increase in sleep and decrease in activity) and prior COVID-19 infection status in the first dose or vaccine type (Moderna versus Pfizer/BioNTech) in the second dose, which have also been previously reported to correlate with subjective symptoms. These early findings show that it is possible to detect subtle, but important changes from an individual’s normal as objective evidence of reactogenicity, which, with further work, could prove useful as a surrogate for vaccine-induced immune response.
References
- Quer, G., et al. Inter-individual variation in objective measure of reactogenicity following COVID-19 vaccination via smartwatches and fitness bands. npj Digital Medicine 5, 49 (2022).
- Quer, G., et al. Wearable sensor data and self-reported symptoms for COVID-19 detection. Nature Medicine 27, 73-77 (2021).
- Quer, G., Gouda, P., Galarnyk, M., Topol, E.J. & Steinhubl, S.R. Inter- and intraindividual variability in daily resting heart rate and its associations with age, sex, sleep, BMI, and time of year: Retrospective, longitudinal cohort study of 92,457 adults. PloS one 15, e0227709 (2020).
- Gadaleta, M., et al. Passive detection of COVID-19 with wearable sensors and explainable machine learning algorithms. NPJ Digit Med 4, 166 (2021).
- Radin, J.M., et al. Assessment of Prolonged Physiological and Behavioral Changes Associated With COVID-19 Infection. JAMA Network Open 4, e2115959-e2115959 (2021).
- Presby, D.M. & Capodilupo, E.R. Biometrics from a wearable device reveal temporary effects of COVID-19 vaccines on cardiovascular, respiratory, and sleep physiology. Journal of Applied Physiology 132, 448-458 (2022).
- Mason, A.E., et al. Metrics from Wearable Devices as Candidate Predictors of Antibody Response Following Vaccination against COVID-19: Data from the Second TemPredict Study. Vaccines 10, 264 (2022).
Follow the Topic
-
npj Digital Medicine

An online open-access journal dedicated to publishing research in all aspects of digital medicine, including the clinical application and implementation of digital and mobile technologies, virtual healthcare, and novel applications of artificial intelligence and informatics.
Related Collections
With Collections, you can get published faster and increase your visibility.
Evaluating the Real-World Clinical Performance of AI
Publishing Model: Open Access
Deadline: Jun 03, 2026
Impact of Agentic AI on Care Delivery
Publishing Model: Open Access
Deadline: Jul 12, 2026

Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in