Real-world evaluation of cinacalcet on hard outcomes in hemodialysis patients in Saudi Arabia
Published in Biomedical Research
Among the tools used to manage SHPT, cinacalcet, a calcimimetic drug, has generated both excitement and debate. While it effectively improves laboratory markers like parathyroid hormone (PTH), calcium, and phosphate levels, its ability to impact “hard outcomes” such as heart attacks, hospitalizations, and survival has remained uncertain.
Recently, my colleagues and I set out to examine this question in a Saudi Arabian population of patients with CKD on hemodialysis. The results, now published in BMC Nephrology, offer valuable real-world evidence that may guide clinicians in the region and beyond.
Why Focus on Cinacalcet and Saudi Patients?
Saudi Arabia faces a rising burden of kidney disease. Diabetes and hypertension—the two leading causes of CKD worldwide—are highly prevalent in the Kingdom. This makes CKD not only a medical problem but also a public health and economic challenge.
Although many international studies have evaluated cinacalcet, very few have looked specifically at its impact in Middle Eastern populations. Moreover, most earlier studies concentrated on biochemical improvements rather than patient-centered outcomes like heart attacks or survival.
As clinicians and researchers based in Saudi hospitals, we felt it was critical to close this evidence gap. Could cinacalcet provide tangible benefits to Saudi patients beyond lab values? Could it reduce cardiovascular complications and hospitalizations, which are both devastating for patients and costly for the healthcare system?
The Study Design: Mixing Retrospective and Prospective Approaches
We designed a multicenter cohort study across three hospitals in the Eastern Province of Saudi Arabia. Our study period spanned December 2019 to January 2021 and combined both retrospective and prospective elements.
Why this hybrid design? When we began, the retrospective sample alone did not yield enough patients to achieve sufficient statistical power. By adding a prospective phase, we were able to enlarge the cohort and strengthen the validity of our findings.
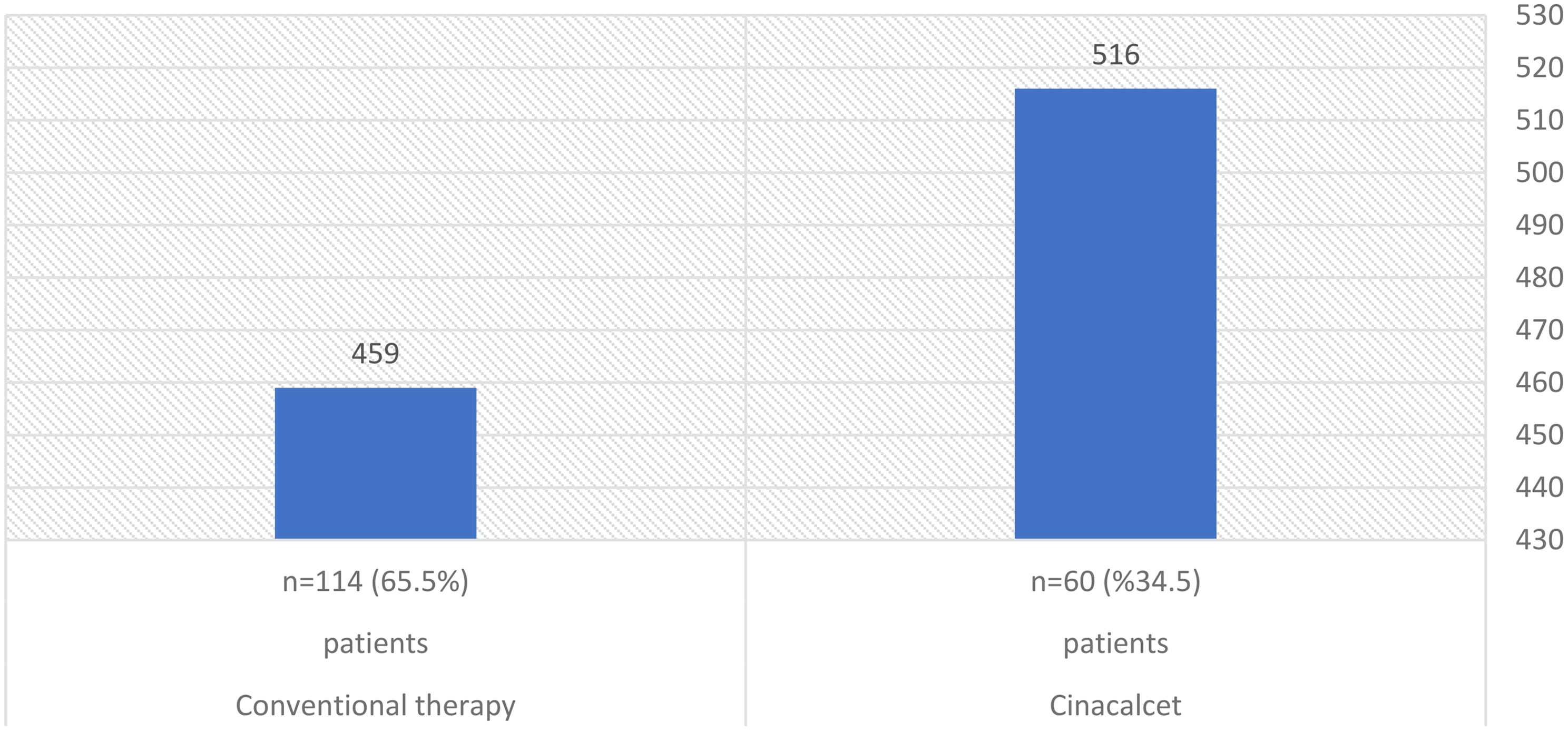
A total of 174 patients were included. Among them, 60 received cinacalcet in addition to conventional therapy (vitamin D analogs, phosphate binders, and dietary modifications), while 114 received conventional therapy alone. All patients were followed for a median of 12 months.
This setup allowed us to compare real-world outcomes between groups while capturing the diversity of patients encountered in daily practice.
Key Findings: Cardiovascular Benefits but Limited Survival Gains
Our results provided a nuanced picture:
Fewer Cardiovascular Events: Patients taking cinacalcet experienced significantly fewer cardiovascular complications. Specifically, the risk of coronary artery disease events such as unstable angina and myocardial infarction was reduced by 61%. This is a striking finding, considering that cardiovascular disease accounts for the vast majority of deaths in dialysis patients.
Reduced Hospitalizations: Cinacalcet was associated with a 69% reduction in the risk of first hospitalization from any cause. This highlights its potential to not only improve patient health but also reduce strain on hospital resources.
No Overall Survival Advantage: When looking at all-cause and cardiovascular mortality, cinacalcet did not significantly improve survival across the entire cohort. However, in patients whose CKD was caused by hypertension or a combination of diabetes and hypertension, cinacalcet was associated with a survival benefit. This suggests that specific subgroups may derive more benefit than others.
Bone Health: The incidence of bone fractures was not significantly different between groups. Yet, a protective trend appeared in older patients and males, though this did not reach statistical significance.
Behind the Scenes: Conducting the Research
Conducting this study was both rewarding and challenging. Our team relied heavily on electronic medical records, dialysis department logs, and input from nephrologists, which required meticulous data cleaning and harmonization to ensure accuracy across three different centers. Because cinacalcet was relatively new to the local hospital formulary at the time, we were able to clearly identify new users, providing a precise baseline for analysis—an advantage often missing in retrospective-only studies. Given that the data were not normally distributed, we applied non-parametric tests such as the Mann–Whitney U and chi-square tests, and employed Kaplan–Meier survival curves alongside Cox proportional hazards models to adjust for confounders including age, gender, PTH levels, and underlying CKD cause. Nonetheless, as with all observational studies, confounding cannot be entirely ruled out, and the 12-month follow-up period was relatively short to fully assess long-term outcomes such as mortality and fractures.
Challenges and Emotional Realities
Conducting research in dialysis centers is both professionally rewarding and emotionally taxing. During the study, 34 patients passed away, underscoring the high mortality inherent in this population. Researchers and healthcare providers must prepare for the emotional impact of such work. Strategies include building emotional resilience, seeking peer support, maintaining professional boundaries, practicing self-care, and focusing on the broader purpose of improving patient care. Acknowledging the human experience behind the data enhances the ethical and emotional foundation of research, fostering compassion alongside scientific rigor.
Why These Results Matter?
Our study is the first in Saudi Arabia to comprehensively evaluate the clinical outcomes of cinacalcet in patients with SHPT on dialysis.
The findings have several implications:
Clinical Practice: Nephrologists may consider cinacalcet not only for its biochemical effects but also for its ability to reduce cardiovascular events and hospitalizations.
Patient Subgroups: Special attention should be paid to patients with hypertension or diabetes plus hypertension, who may gain survival benefits from cinacalcet therapy.
Healthcare Systems: Fewer hospitalizations translate into reduced healthcare costs and resource utilization, a critical consideration in settings where dialysis services already strain budgets.
The Broader Debate: Lessons from EVOLVE and Beyond
Cinacalcet’s role in clinical outcomes has been debated for over a decade, especially after the EVOLVE trial in 2012 failed to show a clear survival advantage. Critics pointed to baseline imbalances and high dropout rates as possible explanations. Subsequent post-hoc analyses suggested that cinacalcet may indeed reduce certain cardiovascular outcomes, especially in older patients.
Our real-world findings contribute to this ongoing conversation. By focusing on an understudied population, we add evidence that cinacalcet may provide tangible benefits—even if not uniformly across all patient groups.
Looking Forward
This research is not the final word on cinacalcet but rather a stepping stone.
Future directions could include:
Larger, longer-term studies to confirm survival effects in specific subgroups.
Comparative studies of cinacalcet with newer agents.
Exploration of cost-effectiveness, given the dual burden of high CKD prevalence and limited healthcare resources in the Middle East.
Conclusion
In summary, our study revealed that cinacalcet reduces cardiovascular events and hospitalizations among Saudi hemodialysis patients with SHPT. While it did not improve overall survival, a benefit was observed in patients with hypertension-related CKD.
These findings highlight the importance of real-world evidence in complementing clinical trials and tailoring therapies to local populations. For clinicians, policymakers, and patients alike, the message is clear: cinacalcet remains a valuable tool in managing one of CKD’s most dangerous complications.
Follow the Topic
-
BMC Nephrology

This is an open access journal publishing original peer-reviewed research articles in all aspects of the prevention, diagnosis and management of kidney and associated disorders, as well as related molecular genetics, pathophysiology, and epidemiology.
Related Collections
With Collections, you can get published faster and increase your visibility.
Robotic surgery: clinical application in nephrology
BMC Nephrology is calling for submissions to our Collection on Robotic surgery: clinical application in nephrology.
Robotic surgery has emerged as a transformative approach in the field of nephrology, enabling surgeons to perform complex procedures with enhanced precision and control. With the advent of advanced robotic systems, such as the da Vinci Surgical System, urologists are now able to tackle intricate renal surgeries that were previously deemed challenging with traditional methods. As the technology continues to evolve, its applications in nephrology are expanding, paving the way for innovative surgical practices.
The integration of robotic surgery into nephrology is of critical importance as it addresses the increasing demand for effective and less invasive treatment options for renal diseases. Recent advancements in robotic technology have led to improved dexterity and visualization during surgery, allowing for greater surgical accuracy. The continuous development in this field not only promises enhanced surgical outcomes but also positions robotic surgery as a key player in the future of renal care.
Topics of interest include, but are not limited to:
Applications of da Vinci surgery in nephrology
Innovations in robotic microsurgery
High-tech surgery techniques in renal procedures
Future directions in robotics in medicine
This Collection supports and amplifies research related to SDG 3 (Good Health and Well-being) and SDG 9 (Industry, Innovation, and Infrastructure).
All manuscripts submitted to this journal, including those submitted to collections and special issues, are assessed in line with our editorial policies and the journal’s peer review process. Reviewers and editors are required to declare competing interests and can be excluded from the peer review process if a competing interest exists.
Publishing Model: Open Access
Deadline: May 22, 2026
Novel therapies for glomerular diseases
BMC Nephrology invites submissions to our Collection on Novel therapies for glomerular diseases.
Glomerular diseases encompass a diverse group of disorders that affect the kidney's filtering units, leading to significant morbidity and mortality. These conditions, which include focal segmental glomerulosclerosis, minimal change disease, and IgA nephropathy, have traditionally posed challenges in terms of effective treatment options. Recent advancements in our understanding of the underlying pathophysiology and the introduction of novel therapeutic modalities, such as targeted biologics and small molecules, present new avenues for intervention. This Collection invites contributions that explore these innovative therapies and their potential to transform the management of glomerular diseases.
Advances in clinical research have led to promising developments, including the successful completion of several clinical trials that evaluate the efficacy of new agents. These therapies not only aim to improve patient outcomes but also focus on personalized treatment approaches that consider individual patient characteristics. By fostering collaboration among researchers, clinicians, and industry partners, we can enhance our understanding and management of these complex conditions. Continued research in this field has the potential to yield groundbreaking discoveries that could redefine treatment paradigms for glomerular diseases.
Topics of interest for this Collection include, but are not limited to:
Novel therapeutic agents in glomerular diseases
Clinical trials of innovative treatments
Impact of new therapies on patient outcomes
Personalized treatment approaches for glomerular disorders
This Collection supports and amplifies research related to SDG 3: Good Health and Well-being and SDG 9: Industry, Innovation, and Infrastructure.
All manuscripts submitted to this journal, including those submitted to collections and special issues, are assessed in line with our editorial policies and the journal’s peer review process. Reviewers and editors are required to declare competing interests and can be excluded from the peer review process if a competing interest exists.
Publishing Model: Open Access
Deadline: Jun 30, 2026


Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in