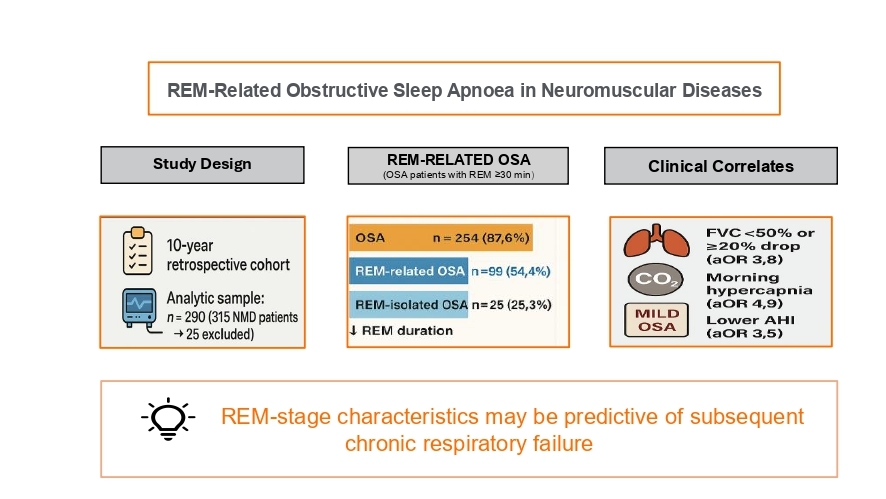
REM-related obstructive sleep apnoea in neuromuscular diseases: A 10-year retrospective cohort study
Published in Biomedical Research
Neuromuscular diseases (NMDs) are frequently accompanied by sleep-disordered breathing, with important consequences for morbidity, quality of life, and survival. Although nocturnal hypoventilation is often considered the dominant problem in NMD and may first appear during REM sleep, obstructive sleep apnoea (OSA) is also encountered in this population. REM sleep is a physiologically vulnerable stage: muscle atonia reduces intercostal activity and upper-airway dilator tone, increasing airway resistance. In NMD, diaphragmatic weakness and pharyngeal instability may further increase susceptibility to obstructive events. Despite this clinical rationale, the prevalence of REM-related OSA and its correlates in NMD have been unclear, and definitions have varied across studies.
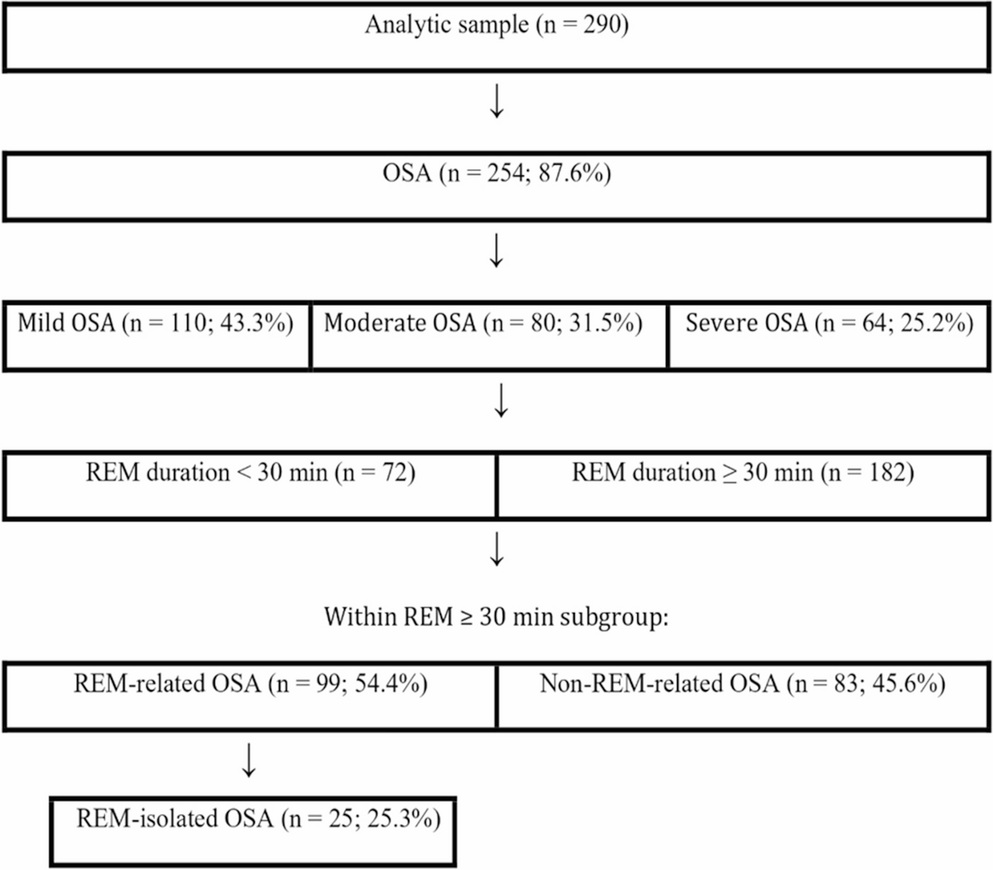
To address this gap, we retrospectively reviewed adults with confirmed NMD who underwent overnight polysomnography between 2015 and 2024. We collected demographic characteristics, comorbidities, polysomnographic indices, spirometry (upright and supine where available), and morning arterial blood gases. We applied a commonly used definition of REM-related OSA (overall AHI ≥5 events/hour, REM-to-NREM AHI ratio ≥2, and REM duration ≥30 minutes). A more specific subgroup, REM-isolated OSA, additionally required NREM AHI <5 events/hour. For between-group analyses, we focused on patients with OSA and REM sleep ≥30 minutes, comparing REM-related versus NREM-related OSA.
Three findings were particularly striking. First, REM sleep was markedly reduced in this NMD cohort, yet OSA was highly prevalent. Among 290 patients, OSA was present in 87.6% (254/290). Mean REM sleep was 11.8% of total sleep time (46.8 minutes), and 30.0% of patients had REM duration <30 minutes. Second, among OSA patients with REM ≥30 minutes (n=182), REM-related OSA was common (54.4%), and 25.3% met criteria for REM-isolated OSA. Third, the REM-related phenotype had clinically meaningful associations. Compared with NREM-related OSA, patients with REM-related OSA tended to have a lower overall AHI with severe OSA being uncommon, but they showed worse REM oxygenation and a substantially higher prevalence of morning hypercapnia.
In multivariable models, REM-related OSA remained independently associated with morning hypercapnia (aOR 4.889), significant respiratory muscle weakness (FVC <50% predicted and/or ≥20% upright-to-supine FVC decline; aOR 3.847), and mild OSA (aOR 3.461). These findings support the idea that REM-stage abnormalities may act as early markers of evolving respiratory failure in NMD, even when “global” OSA severity appears mild.
We hope these results encourage clinicians to look beyond overall AHI and to assess REM duration, REM/NREM distribution of events, and REM-specific oxygenation when interpreting PSG in NMD. Prospective longitudinal studies are needed to determine whether REM-related OSA severity changes over time and to quantify therapeutic responses to positive airway pressure strategies.
Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in