Roles and expenses of self-care behaviours for tackling type 2 diabetes in developing countries
Published in General & Internal Medicine and Public Health
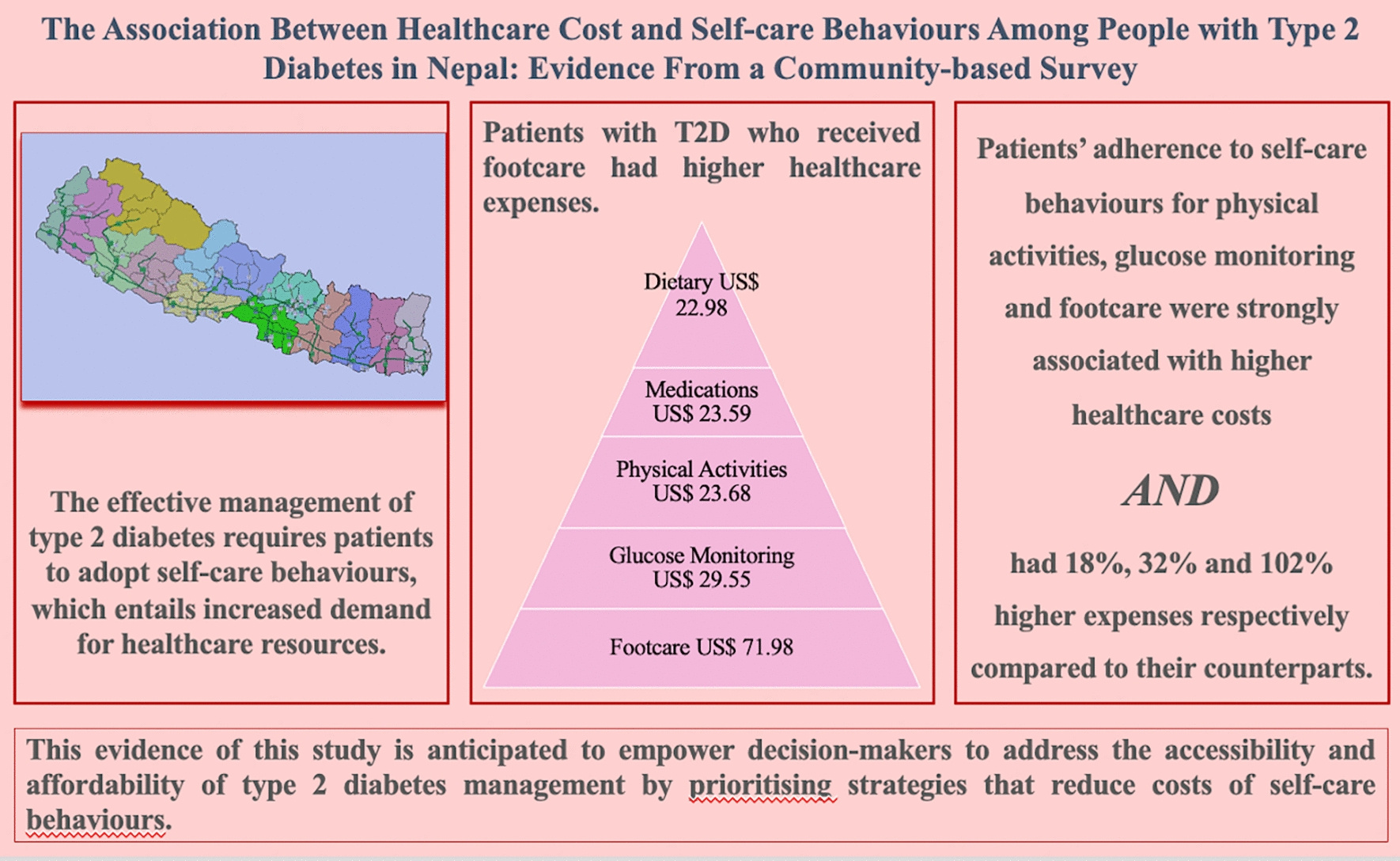
Developing countries face unique challenges in managing T2DM, where the disease imposes significant financial strain on patients. The direct costs include medications, regular medical consultations, and hospitalisations, while indirect costs cover lost productivity, transportation to healthcare facilities, and long-term complications. For many patients, these expenses are overwhelming, leading to inadequate disease management and poorer health outcomes. Our recent research, published in Discover Health Systems, explores the healthcare costs associated with Type 2 diabetes mellitus (T2DM) across various self-care behaviours and highlights the critical role these behaviours play in effective disease management.
Evidence shows that self-care behaviours are pivotal in managing T2DM effectively. These include regular physical activity, which helps maintain blood glucose levels and overall health; dietary adherence, where following a balanced diet can prevent blood sugar spikes and manage weight; and medical adherence, where consistent medication use ensures optimal blood glucose control. Additionally, glucose monitoring, through regular blood sugar checks, helps patients make informed decisions about their care, and foot care prevents complications like infections and ulcers, which can lead to severe outcomes if untreated.
Our study focused on analysing the healthcare costs associated with these self-care behaviours among T2DM patients, and the findings are revealing. Foot care emerged as the most expensive self-care behaviour, despite being the least practiced. Foot complications can lead to severe outcomes, including amputations, significantly raising healthcare costs. Glucose monitoring was also a high-cost behaviour, essential for preventing long-term complications but often neglected due to financial constraints. Physical activity, while crucial for maintaining health, faces barriers in cost and accessibility of facilities and safe environments for exercise. This research underscores the need for strategies to make these self-care behaviours more affordable and accessible. By addressing these barriers, we can improve T2DM management and outcomes for patients in developing countries.
Our findings provide valuable insights for policymakers, healthcare practitioners, and patients. Policymakers must prioritise funding and initiatives that reduce the cost of essential self-care behaviours. Subsidies for glucose monitoring, affordable footwear, and community exercise programs could alleviate the economic burden on patients. Healthcare practitioners should emphasise the importance of comprehensive self-care in diabetes management, educating patients about cost-effective strategies and available resources to enhance adherence to these practices. Patients should be encouraged to incorporate affordable self-care practices into their daily routines, with community support groups and educational programs playing a crucial role in this effort.
Managing T2DM in developing countries requires a multifaceted approach that addresses the economic barriers to effective self-care. Our research highlights the significant costs associated with essential self-care behaviours and the urgent need to make these practices more accessible and affordable. By doing so, we can improve health outcomes and reduce the financial burden on patients, ultimately enhancing the quality of life for those living with type 2 diabetes.
Our research not only highlights the economic challenges faced by T2DM patients but also provides a roadmap for stakeholders to implement changes that can lead to better disease management. Ensuring that self-care behaviours are affordable and accessible is a critical step toward reducing the prevalence and impact of type 2 diabetes in developing countries. For details https://link.springer.com/article/10.1007/s44250-024-00117-2.
Follow the Topic
-
Discover Health Systems

This journal takes a multidisciplinary approach to address systems-level research and discussions relating to health systems, services and informatics, reflecting health outcomes, including from business and health policy perspectives.
Related Collections
With Collections, you can get published faster and increase your visibility.
Building Resilient Health Systems and Outbreak Preparedness in Africa: Policy, Governance, and Technological Innovation
Achieving timely prevention, detection, and response to infectious disease threats, while maintaining equitable access to essential services—depends on robust, well-governed health systems. In Africa’s diverse contexts, strengthening these systems requires integrated policy frameworks, adaptive management practices, and innovative technologies that address gaps in surveillance, workforce capacity, supply chains, and community engagement.
This Article Collection examines multidisciplinary strategies to enhance health system resilience and epidemic preparedness across the continent. We focus on:
- Policy and Governance: Crafting adaptive national and subnational policies, financing models, and regulatory environments that incentivize rapid outbreak response and sustain routine care.
- Health System Management: Optimizing human resources for health, supply-chain logistics, and facility-level coordination to maintain continuity of care during emergencies.
- Digital Health & Informatics: Deploying electronic surveillance platforms, mobile health (mHealth) tools, and data-analytics dashboards for real-time monitoring, early warning, and evidence-based decision-making.
- Surveillance & Laboratory Networks: Expanding laboratory capacity, sample-transport systems, and integrated One Health approaches to detect zoonoses and emerging pathogens.
- Community Engagement & Risk Communication: Leveraging regional partnerships, local governance, and culturally tailored messaging to build trust and promote preventive behaviors.
- Operational Research & Evaluation: Implementing outbreak simulations, performance metrics, and rapid-cycle evaluations to refine interventions and inform scalable best practices.
We welcome submissions that generate practical, scalable solutions for African health systems. By uniting insights from policymakers, health managers, informaticians, and frontline practitioners, this Collection aims to inform evidence-driven investments, strengthen preparedness capacities, and improve health outcomes across the continent.
Publishing Model: Open Access
Deadline: Jun 01, 2026
Improving Domestic resource mobilisation to support health financing transition in Sub-Saharan Africa
It is generally acknowledged that recent improvements in health outcomes in Africa have been attributed to the increase in development assistance for health, especially over the past three decades. With development assistance for health in Sub-Saharan Africa on the decline, increased domestic resource mobilization for health will be needed to sustain progress or even avoid disruptions, given recent and likely future declines in external support.
There is also a general recognition that bridging the funding gap in the face of declining donor aid funding will depend crucially on governments in Africa increasing domestic funding and planning transitions towards greater domestic health spending. Arguably, recent events in the global health financing architecture have only added impetus to a situation that has been unfolding for several years. Despite high-level political and policy statements, domestic financing remains very low in many African countries.
Thus, one question that confronts national health authorities and health financing policy experts is, are there plausible scenarios over the short and medium term to transition towards increased domestic financing in anticipation of declining development assistance for health, with minimal disruptions to the progress made so far? Rather than focusing on aspirational targets, such as the share of total government spending allocated to the health sector, it is essential to examine how well countries are performing, given their level of income and other spending drivers. Bringing new evidence on the potential of African countries to increase domestic resources for health into one collection would greatly add value to the debate.
This collection will feature empirical papers that will hopefully examine the extent to which countries can increase domestic resources for health. The scope of empirical papers covers the following pertinent dimensions of health financing, including revenue mobilization, risk pooling, and strategic purchasing:
(a) Quantifying the potential for domestic resource mobilization for health
(b) Modelling future health spending and costs in the short to medium term, incorporating scenarios about anticipated changes in external health financing.
(c) Estimating the efficiency or effectiveness of health spending.
(d) Evaluating the impact of strategic purchasing on health system performance
(e) Description and evaluation of levels and patterns of development assistance for health in sub-Saharan Africa.
(f) Evaluation of effective strategies that countries are implementing to increase domestic financing for health.
Publishing Model: Open Access
Deadline: Aug 26, 2026

Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in