Salivary and serum leptin levels in oral lichen planus patients. A case control study
Published in General & Internal Medicine
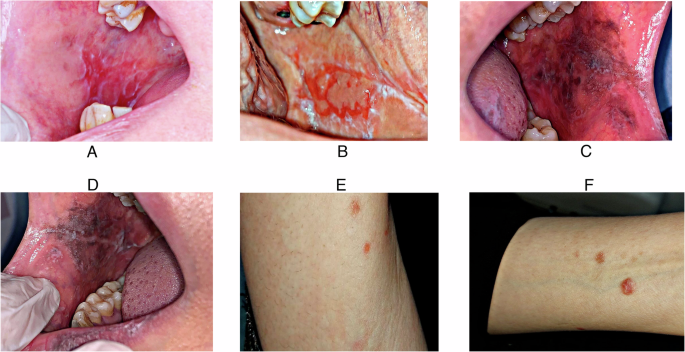
LP is a common condition affecting stratified squamous epithelia. It is a chronic mucocutaneous and immunological illness with a variety of clinical symptoms. The oral mucosa is frequently affected, and in rare cases, it may be the only site of involvement. OLP can appear in six different clinical forms: reticular, papular, plaque-like, atrophic (erythematous), erosive-ulcerative, and bullous-erosive. The buccal mucosa is the most impacted area, followed by the lingual, gingival, and labial mucosa. Wickham striae, which are white hyperkeratotic papules that give the lesions a lace-like look, are a defining feature of OLP.
White adipose tissue secretes the polypeptide hormone leptin, which has been connected to dyslipidemia in LP and is involved in immunological responses. Research has consistently shown a relationship between greater body mass index (BMI), increased body fat, and heightened leptin levels. Additionally, leptin promotes autoimmune and cellular immune responses. Assessing the diagnostic value of serum and salivary leptin levels in OLP was the aim of the current investigation.
The study included 39 patients with OLP and 39 control subjects, were chosen from the outpatient clinic of the Department of Oral Medicine, Periodontology, and Oral Diagnosis at Cairo University's Faculty of Dentistry for the study. Clinicaltrials.gov is where the study protocol was registered (NCT06078579). The research was carried out between December 2023 and September 2024. This study was conducted in accordance with the Declaration of Helsinki and adheres to the CONSORT declaration.
Selection of Subjects:
Criteria for Inclusion: The age range for both sexes is 30 to 70, Histological confirmation and clinical diagnosis have been obtained for symptomatic OLP.
After being fully informed about the study, participants sign a written consent form.
Exclusion criteria: Using a systemic or locally administered medication within three months of the start of the study may change how inflammatory mediators are expressed in the tissue,
NSAID users may have alterations in tissue expression of inflammatory mediators if they are currently taking them or have recently stopped using them, Individuals who have been diagnosed with cancerous tumors, Individuals who are nursing or pregnant, The aged, mentally ill, prisoners, and others fall under this category.
The American Academy of Oral and Maxillofacial Pathology's clinical and histological criteria were used to establish the diagnosis of oral lichen planus. Clinically, the lesions showed up on both sides with the usual white striae of the reticle, frequently with erosive or atrophic patches. Histopathologically, the tissues displayed basal cell degeneration together with a band-like lymphocytic infiltration in the superficial connective tissue.
Degeneration of basal cells and lymphocytic infiltration in the superficial connective tissue. The three types of oral lesions were bullous-erosive, reticular, and atrophic. A clinical examination was performed on the patients, utilizing natural light for skin lesions and a spotlight and magnifying glass for oral lesions. The clinical diagnosis was conclusively confirmed by the discovery of Wickham's striae. These striae, which cannot be eliminated by rubbing, would be highlighted by stretching the mucosa on the surface.
The subject's or patient's name, age, gender, the date of the lesions' initial diagnosis, and their medical and dental history were all gathered at the initial evaluation. The researchers performed clinical oral examinations and collected baseline data. The amount and location of mucosal/cutaneous lesions, disease severity levels, and the biopsy site were among the demographic, clinical, and laboratory data that they photographed for every patient in the two study groups. The diagnosis was later confirmed by biopsy.
The OLP group's observed salivary leptin levels were substantially greater than the controls' (p<0.001) when compared across groups. The OLP group's mean salivary leptin levels were 15.31±6.59, while the control group's mean salivary leptin levels were 4.90±1.26. These findings point to a potential function of salivary leptin as a diagnostic biomarker as well as a part in the pathophysiology of OLP.
The OLP group had considerably greater serum leptin levels than the control group (p < 0.001). The OLP group's mean serum leptin level was 13.23 ± 7.29 ng/mL, while the control group's was 4.20 ± 1.23 ng/mL. Similar results were documented, confirming serum leptin's potential as a diagnostic biomarker and its involvement in the pathophysiology of OLP.
Salivary and serum leptin levels showed a statistically significant strong positive connection (rₛ = 0.890, p < 0.001). These results underline the potential of salivary and serum leptin as diagnostic biomarkers for OLP by indicating that they both contribute equally to the pathophysiology of the disorder.
Follow the Topic
-
British Dental Journal

This is an international, peer-reviewed journal for the dental community, published by Springer Nature on behalf of the British Dental Association.
Related Collections
With Collections, you can get published faster and increase your visibility.
Periodontology
Publishing Model: Hybrid
Deadline: Jun 30, 2026




Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in