Selection of Treatment Options for Locally Advanced Rectal Cancer: An MRI-based Risk Stratification Scoring System
Published in Cancer
Locally advanced rectal cancer (LARC) is one of the most devastating cancers worldwide, with substantial recurrence rates despite standard treatments. The search for the optimal neoadjuvant treatment strategy for LARC has been ongoing and evolving over time. However, these treatments tested in clinical trials may lead to unwanted side effects, such as late neurotoxicity or a breached mesorectum. Hence, it is crucial to have a scoring system that can differentiate between high-risk and low-risk recurrence in rectal cancer patients before treatment. Such a system facilitates more meaningful discussions between clinical decision-makers and patients regarding the potential risks and benefits of treatment. Magnetic resonance imaging (MRI) has become the most standardized approach for defining the locoregional clinical staging of rectal cancer and plays a pivotal role in determining the success of selected treatment strategies. However, the absence of uniform MRI criteria hinders clinicians in making precise clinical decisions for different neoadjuvant treatment strategies. Therefore, our objective was to develop a scoring system using MRI markers for rectal cancer to discriminate between patients at high risk of recurrence and those at low risk.
To establish the scoring system, we conducted a multicenter observational study that enrolled patients with rectal cancer who received neoadjuvant chemoradiotherapy (nCRT). The study comprised two cohorts: Cohort 1, which was retrospectively recruited from five hospitals in China, and Cohort 2, a retrospective analysis of a previous prospective trial (No. NCT04271657). The sample size was determined based on the number of cases in these areas during the study period. The study evaluated two primary outcomes in Cohort 1: the 3-year disease-free survival (DFS) and 5-year overall survival (OS). In addition, the pathologists examined the histopathological TRG as a marker of nCRT response in Cohort 1 and Cohort 2.
The radiologists evaluated several imaging makers derived from pelvic MRI in rectal cancer, including the mrN and mrT stage, mrTDs (tumor deposit), mrEMVI (extramural vascular invasion), and mrCRM (circumferential resection margin). MRI imaging markers were evaluated and measured by two radiologists with more than 5 years and less than 10 years experiences in interpreting abdominal imaging. In the event of disagreement, the final decision was made by an arbitration expert, a senior radiologist with over 10 years of experience. Subsequently, we attempted to establish a scoring system to complement the TNM staging system and evaluate the risk of recurrence in LARC patients. The system incorporated three MRI markers to achieve this objective, including mrCRM, mrEMVI, and mrTDs. Each marker was assigned a score of 1 for positive and 0 for negative, and then these scores were accumulated to create the mrDEC scoring system. The range of scores was from 0 (when all three MRI markers were negative) to 3 (when all three MRI markers were positive). With this scoring system, patients were categorized into four risk groups: low-risk (score = 0), intermediate-low-risk (score = 1), intermediate-high-risk (score = 2), and high-risk (score = 3). The entire workflow of our scoring system is presented in Fig. 1.
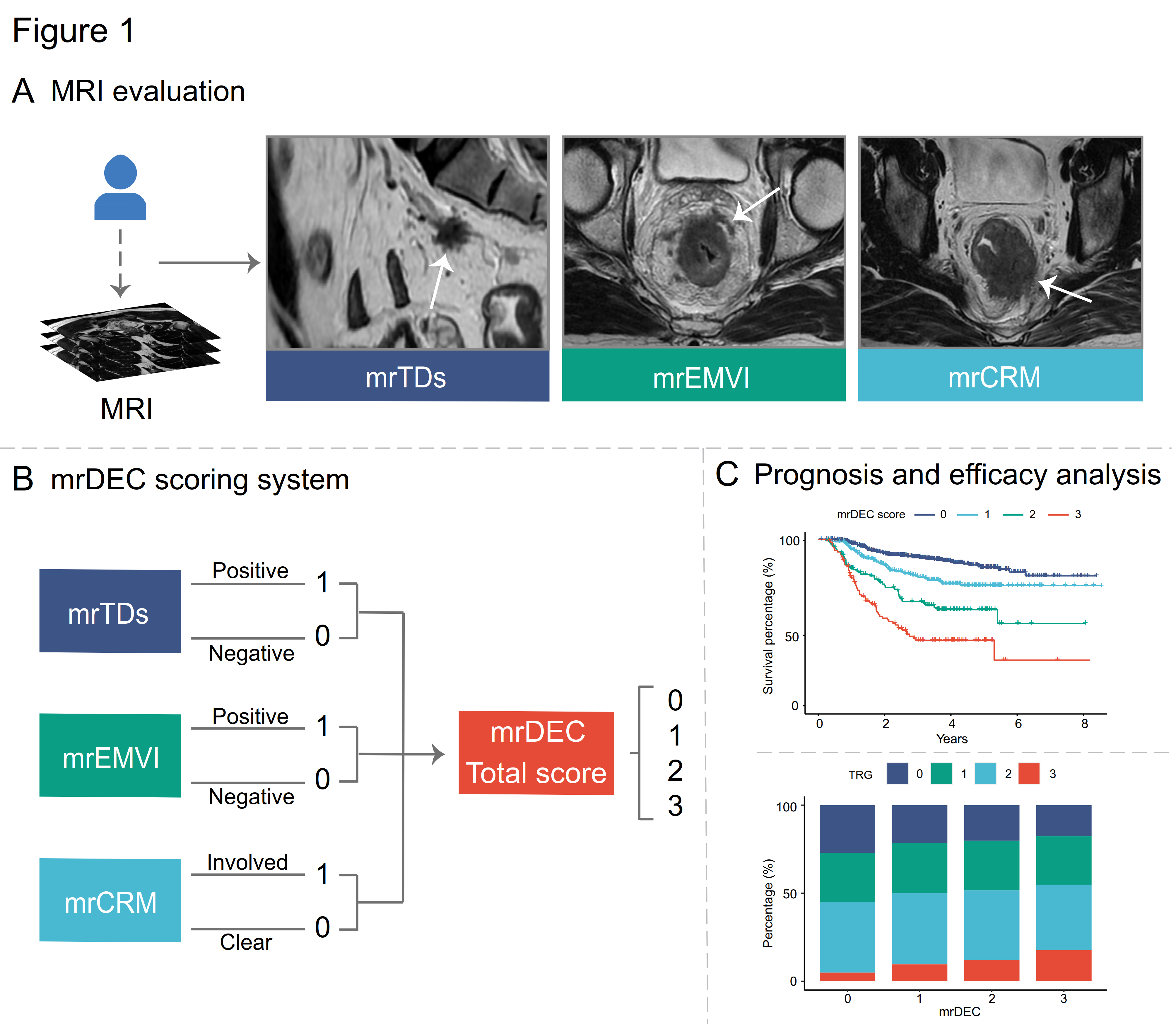
Figure 1. Evaluation workstreams and construction of scoring system.
(A) Evaluation of rectal cancer magnetic resonance image. (B) The construction of the mrDEC scoring system. (C) Prognosis and efficacy analysis according to mrDEC score. mr, magnetic resonance; TD, tumor deposit; EMVI, extramural vascular invasion; CRM, circumferential resection margin; TRG, tumor regression grade.
We validated this mrDEC scoring system in Cohort 1 and found that the 3-year DFS for a total score of 0 to 3 was 91.0%, 79.5%, 65.5%, and 44.0%, respectively. Patients with the highest score (total score = 3) had more than seven times the risk of DFS events than those with the lowest score (total score = 0) (9.0% vs. 56%). Moreover, high-risk patients (score = 3) had a worse prognosis than expected (44.0% vs. 79.6%), whereas low-risk patients (score = 0) had a better prognosis than expected (91.0% vs. 79.6%). Given the greater-than-average benefit from traditional nCRT, low-risk patients need no other intensive preoperative treatment therapies to avoid unwanted side effects. The OS showed the same trend, with high-risk patients having a worse prognosis than expected (44.5% vs. 84.8%) and low-risk patients having a better prognosis than expected (92.9% vs. 84.8%). Intermediate-low-risk patients (score = 1) and intermediate-high-risk patients (score = 2) require further analysis to determine the needed therapy. Furthermore, in the same therapeutic context, implementing a more intensive surveillance program for high-risk patients is advisable. This approach facilitates the early detection of metastases and promises to improve the prognosis for these individuals.
Furthermore, our study provided evidence that the mrDEC scoring system had strong prognostic ability even when stratified by TRG. This finding is particularly noteworthy given that previous studies have identified the TRG system as an independent predictor of recurrence and survival in patients with LARC who undergo nCRT followed by TME. Specifically, patients with TRG 0 exhibit a significantly better prognosis than those with higher TRG scores, indicating their suitability as candidates for organ-preserving strategies. Interestingly, we observed a negative correlation between the mrDEC score and long-term prognosis in patients with TRG 0. These findings indicated that caution should be exercised when considering an organ-preserving strategy even in patients with high mrDEC scores who achieve TRG 0, as they have a greater risk of a poor prognosis. Consequently, the complementation of mrDEC score system to the existing clinicopathological prognosticators for LARC could provide additional prognostic value.
In conclusion, the mrDEC scoring system developed in this study is a reliable and accurate tool for risk stratifying patients with LARC and determining the need for intensive nCRT. The multicenter validation study demonstrated the prognostic ability of the mrDEC scoring system for patient outcomes, and its prognostic performance surpasses that of single MRI marker. The mrDEC scoring system has the potential to improve treatment decision-making and patient outcomes in clinical practice.
Follow the Topic
-
British Journal of Cancer

This journal is devoted to publishing cutting edge discovery, translational and clinical cancer research across the broad spectrum of oncology.


Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in