Suppressing resistance to cancer therapy
Published in Ecology & Evolution

The paper in Nature Communications is here: http://go.nature.com/2CxCtln
In March 2011, Michael Hochberg from Montpellier’s Institute of Evolutionary Sciences crossed campuses to the Institute of Molecular Genetics to give a seminar advocating a different way of seeing cancer. The evolutionary viewpoint so appealed to cell biologist Dan Fisher that he pitched a collaborative project, which became part of my postdoctoral stint in the Hochberg group, and which culminated in a paper published in Nature Communications last month.
What can a Darwinian perspective offer cancer research? For starters, evolutionary arguments can explain why cancer exists at all, and why cancer risk doesn’t simply correlate with organismal body size and lifespan, nor with the number of cell divisions in a tissue. Patterns of tumour progression and diversification can be understood – potentially even predicted – by considering how natural selection and genetic drift act on expanding populations. And most importantly for patients, evolutionary theory proposes unconventional approaches to cancer prevention and treatment.
The subject of our project was adaptive therapy. As originally formulated, “The goal of adaptive therapy is to enforce a stable tumor burden by permitting a significant population of chemosensitive cells to survive so that they, in turn, suppress proliferation of the less fit but chemoresistant subpopulations.” In eco/evo parlance, this means reducing the fitness of drug sensitive cancer cells while preventing the competitive release of resistant cells, which is the main reason why conventional treatment fails. In clinical terms, the vision is to transform deadly cancers into manageable chronic diseases.
Our aim was to examine how adaptive therapy might work in practice. Does resistance truly incur a fitness cost? How can resistance be suppressed? How much will adaptive therapy benefit patients?
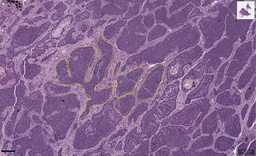
We set about answering these questions through iterated experiments and mathematical modelling. PhD student Katarina Bacevic and her colleagues in the Fisher lab examined interactions between drug sensitive and resistant cells on culture plates and in tumour spheroids, which recapitulate the essential spatial structure of tumours in highly controllable conditions. They also investigated molecular mechanisms of resistance. And every few weeks for three years, I cycled up the hill from my institute to theirs to discuss findings and plan next steps. This continual dialogue enabled me to create mathematical models and computational simulations consistent with experimental protocols and biological understanding of our system. In return, insights from theory ensured that experiments were appropriate for testing the evolutionary assumptions on which adaptive therapy depends.
The experiments confirmed that cancer cells pay a fitness cost for resistance to our candidate adaptive therapy drug and, crucially, spatial structure amplifies this cost. When my colleagues applied just enough drug to halt tumour spheroid growth, the majority drug-sensitive cells effectively constrained proliferation of the minority resistant cells. In contrast, when they applied a higher dose that wiped out the sensitive cells – which is the aim of conventional treatment – the resistant remnants escaped and expanded.
To determine the factors underlying these observations, I created a computational simulation of the tumour spheroid system, which could recapitulate the experimental results. By running many stochastic simulations, I found that the initial spatial distribution of resistance is especially influential. The smaller the distance between the outermost resistant cell and the spheroid’s surface when treatment begins, the lower the chance of successful treatment.
So how much might adaptive therapy extend patient survival, relative to conventional treatment? To obtain some analytical insight, I devised a simple, general mathematical model of tumour evolution. When resistant cell fitness is frequency dependent, the model predicts an upper bound on survival benefit. The limit mostly depends on the relative fitness of resistant cells when they are rare, which in turn depends on their initial spatial distribution. But adaptive therapy may outperform this prediction if it can further manipulate the tumour’s microenvironment, such as by depleting resources or by permitting regrowth of sensitive cells between doses (as another recent study examined in more detail).
In light of our long and close collaboration, my coauthors and I were delighted when a reviewer described our study as “an outstanding example of multidisciplinary research that integrates mathematical modeling with empirical studies”. The reviewer further noted that such cooperation “unfortunately remains rare in cancer.” Intent on overturning the status quo, we’re already planning follow-up experiments and – of course – complementary mathematical modelling.
Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in