Telemedicine-delivered myofunctional therapy induces measurable upper airway remodeling in OSA
Published in Biomedical Research
Obstructive sleep apnea (OSA) is a multifactorial disorder in which upper airway anatomy and neuromuscular control play a decisive role in airway collapsibility during sleep. While continuous positive airway pressure (CPAP) remains the gold standard treatment, it acts as a pneumatic splint and does not directly address the underlying anatomical or functional contributors to airway collapse. As a result, interest has grown in adjunctive therapies capable of modifying these factors.
Myofunctional therapy (MT), based on targeted oropharyngeal exercises, has demonstrated improvements in OSA severity and adherence to other treatments. However, a major limitation in the field has been the lack of objective evidence showing whether MT induces true structural remodeling of the upper airway, particularly when delivered outside traditional face-to-face settings.
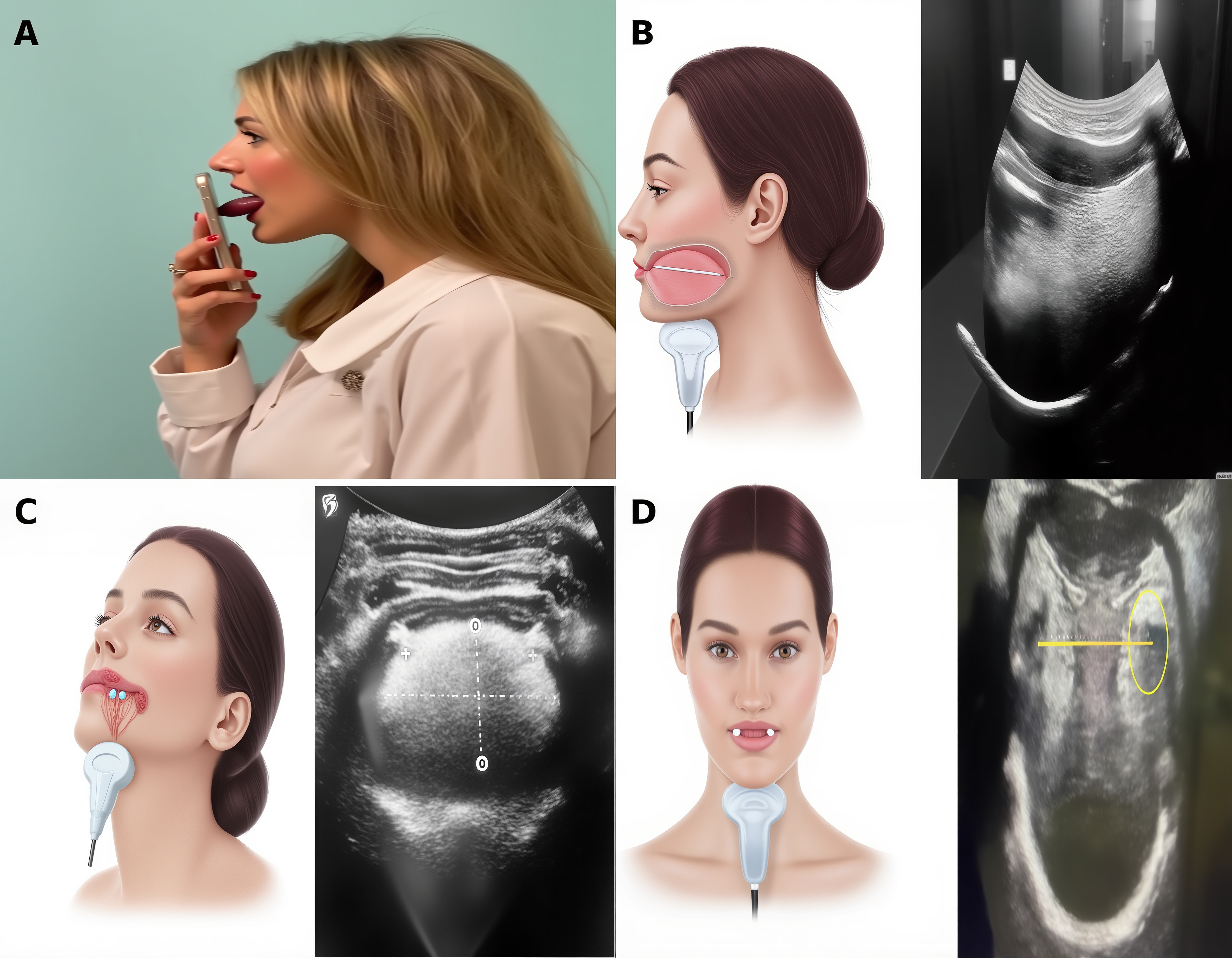
In this prospective controlled study, we evaluated the anatomical and functional impact of MT delivered through a telemedicine platform in patients with moderate-to-severe OSA. By combining submental ultrasound, drug-induced sleep endoscopy (DISE), and objective muscle strength assessment, we were able to assess both static and dynamic changes in the airway. After only three months, patients undergoing telemedicine-based MT showed significant reductions in tongue volume and airway dimensions, accompanied by improvements in tongue base collapse patterns on DISE. No comparable anatomical changes were observed in CPAP-only controls.
Beyond the anatomical findings, this work highlights the potential of telemedicine to enhance adherence, standardization, and scalability of MT programs. Submental ultrasound emerged as a practical, noninvasive tool to monitor airway remodeling over time, offering a feasible imaging biomarker for personalized OSA management.
Together, these results provide objective structural and functional evidence supporting telemedicine-delivered myofunctional therapy as a patient-centered adjunctive strategy in selected OSA phenotypes and open new avenues for integrating imaging-based monitoring into routine clinical practice.
Follow the Topic
-
Clinical Oral Investigations

Clinical Oral Investigations is a multidisciplinary journal for research in oral medicine and maxillofacial science which provides up-to-date results of basic and clinical studies.






Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in