Terrorism in the country of origin is linked to deterioration in the mental health of refugees
Published in Social Sciences

Every year millions of people flee their native country to escape violent conflicts. While some of them make it to a safe haven, and thereby leave behind immediate physical dangers, this does not mean that they are safe from harms from further conflicts in their former country. In our recent paper, we study whether refugees continue to be marred by contemporary terrorism in their country of origin.
One inspiration for the project was previous studies of how immigrants’ and their descendants’ outlooks and behaviors continue to reflect the culture of their ancestral countries. Building off this finding, we hypothesized that refugees’ mental health— as indicated by their use of psychotropic drugs—is continuously adversely affected by contemporary episodes of terrorism in their home countries.
Another inspiration—equally important, but more “practical”—came from one of the authors’ mother, who, as a general practitioner, experienced many refugees consulting her with mental health problems after periods of more pronounced terrorism in their country of origin. This observation from a practician suggested to us that our theoretically motivated hypothesis also has “real-world” resonance.
How did we research this question?
Researching refugees’ mental health is generally very challenging because this group is hard to reach and because mental health is typically studied using “noisy” self-reported indicators. To avoid these pitfalls, we utilized longitudinal population-level registry data from Denmark. These registry data include information on refugee status and country of origin, but also, and more uniquely, time-stamped information about redemption of prescribed psychotropic drugs from pharmacies. Psychotropic drug redemption is a credible “quasi-behavioral” proxy for mental health. If refugees redeem—and, by extension, use—more psychotropic drugs, it is reasonable to assume that this reflects a deterioration in their mental health. In addition, we merge information about casualties from terrorism in refugees’ home countries to gauge their exposure to conflict in this setting.
From our data, we can then examine if contemporary terrorism in refugees’ country of origin is linked to their mental health in terms of their psychotropic drug use. More specifically, we analyze whether refugees are more likely to consume psychotropic drugs that are used in treatment and symptom management of various disorders associated with experiences of psychological trauma (antidepressants, and anxiolytic and hypnotic drugs) in years with higher levels of terrorism in their country of origin in the period 1998-2012. We apply various statistical models to ensure that an observed relationship is not driven by other confounding factors. Perhaps most importantly, we compare within individuals, which effectively means that we compare a given refugee’s psychotropic drug use in a year with more severe terrorism in their country of origin, to her/his own consumption in a year with less severe terrorism in this country.
What do we find?
Our analysis reveals the hypothesized relationship: on average, refugees consume statistically significantly more psychotropic drugs—antidepressants, and anxiolytic and hypnotic drugs—in years with a higher number of casualties in their country of origin compared to years with fewer casualties in that home country. Figure 1 shows the estimated relationship for antidepressants and anxiolytic as well as the distribution of casualties. In substantive terms, an increase from zero to a thousand casualties in a country of origin in a given year—37% of the observations in our data have 1,000 or more casualties—corresponds to a non-trivial increase in psychotropic drug consumption of 5-8 percent depending on the drug type.
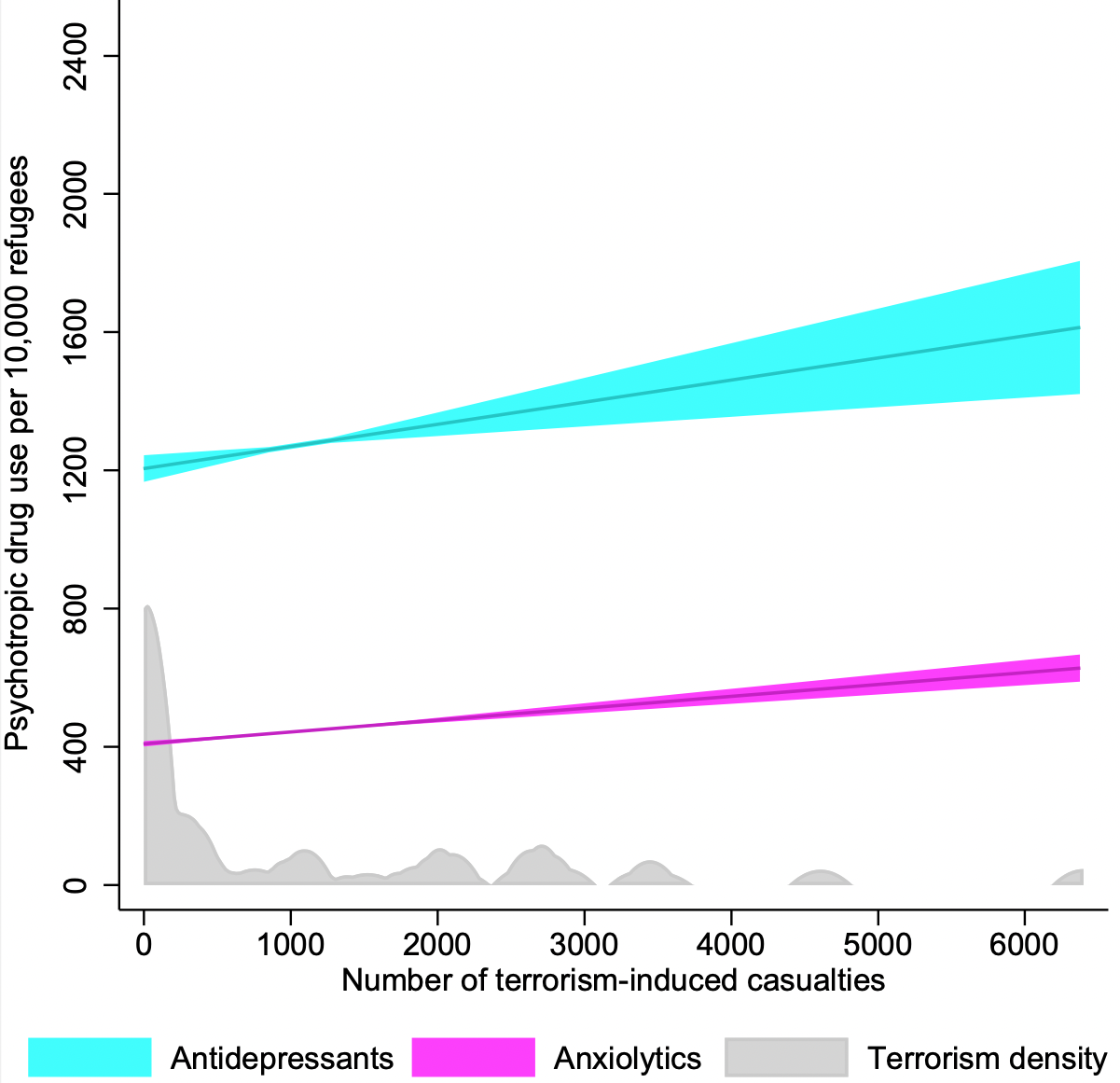
Figure 1: Psychotropic drug use among refugees and casualties from terrorism in country of origin. The figure is based on the estimates in Table 1 in our article (N = 325,337 person-years). The solid lines show the predicted number of refugees (per 10,000 refugees) who redeem antidepressants or anxiolytics at least once in a given year as a function of the number of terrorism-induced casualties in the country of origin. The shaded areas indicate 95% confidence intervals, and the gray area illustrates the distribution of casualties.
We probe this finding in several supplementary analyses. In short, the result is robust to a range of checks and although we cannot claim to have identified a causal relationship in the absence of home-country terrorism being randomly assigned as in an experiment, we can rule out several alternative explanations for the findings.
Why are refugees negatively affected by contemporary terrorism in their country of origin? We can think of at least three potential mechanisms: a rekindling of psychological distress by evoking memories of past trauma (i), a feeling of threat to refugees’ personal relations in their home country (ii), or to their home country more generally (iii). While we cannot firmly adjudicate between these mechanisms, we provide some indirect evidence by repeating our analysis for a related group—(non-refugee) immigrants—who are less likely to have experienced trauma in their country of origin than refugees (because they mostly migrate for different reasons), but likely to hold some of the same personal and symbolic connections to that country. Finding a similar, but weaker relationship between home-country terrorism and psychotropic drug use for this group indicates that at least part of the effect may be driven by a rekindling of past trauma.
Implications: You can run, but you cannot hide
Our finding that contemporary terrorism in the home country is negatively associated with the mental health of refugees highlights the extended global consequences of terrorism as well as the additional vulnerability of a group already at risk. Dishearteningly, those who have fled—specifically from such intimidations—appear to continue to be marred by them. Yet, knowing that this problem exists, and when it is (more) likely to occur, is the first step in ameliorating it—for example, by ensuring that the staff in medical and social services are aware that the mental health of refugees may deteriorate in the event of large-scale terrorist attacks in their home countries, and that extra support and care are therefore needed in such situations.
Image credit: Julie Ricard on Unsplash
Follow the Topic
-
Nature Human Behaviour

Drawing from a broad spectrum of social, biological, health, and physical science disciplines, this journal publishes research of outstanding significance into any aspect of individual or collective human behaviour.



Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in