The Spectrum of Tuberculosis and Why It Matters
Published in Microbiology

TB is an ancient disease that has co-evolved with humans. Despite the decades of research on this disease, we are yet to fully understand the biology of TB and its interactions with the human host.
Classically, two forms of TB have been considered to exist: latent TB infection; and active TB disease. A more recent understanding is that M. tuberculosis infection is associated with a dynamic spectrum of pathology, between adequate containment and progression to active disease.
In a recently published Primer on Tuberculosis in Nature Rev Dis Primers, we provided an overview of our current understanding of the spectrum of TB. Although patients are often categorized as having either latent TB infection or active TB disease for simplicity in clinical and public health settings, there is general acceptance today that individuals can advance or reverse positions, depending on changes in the host immunity and comorbities.
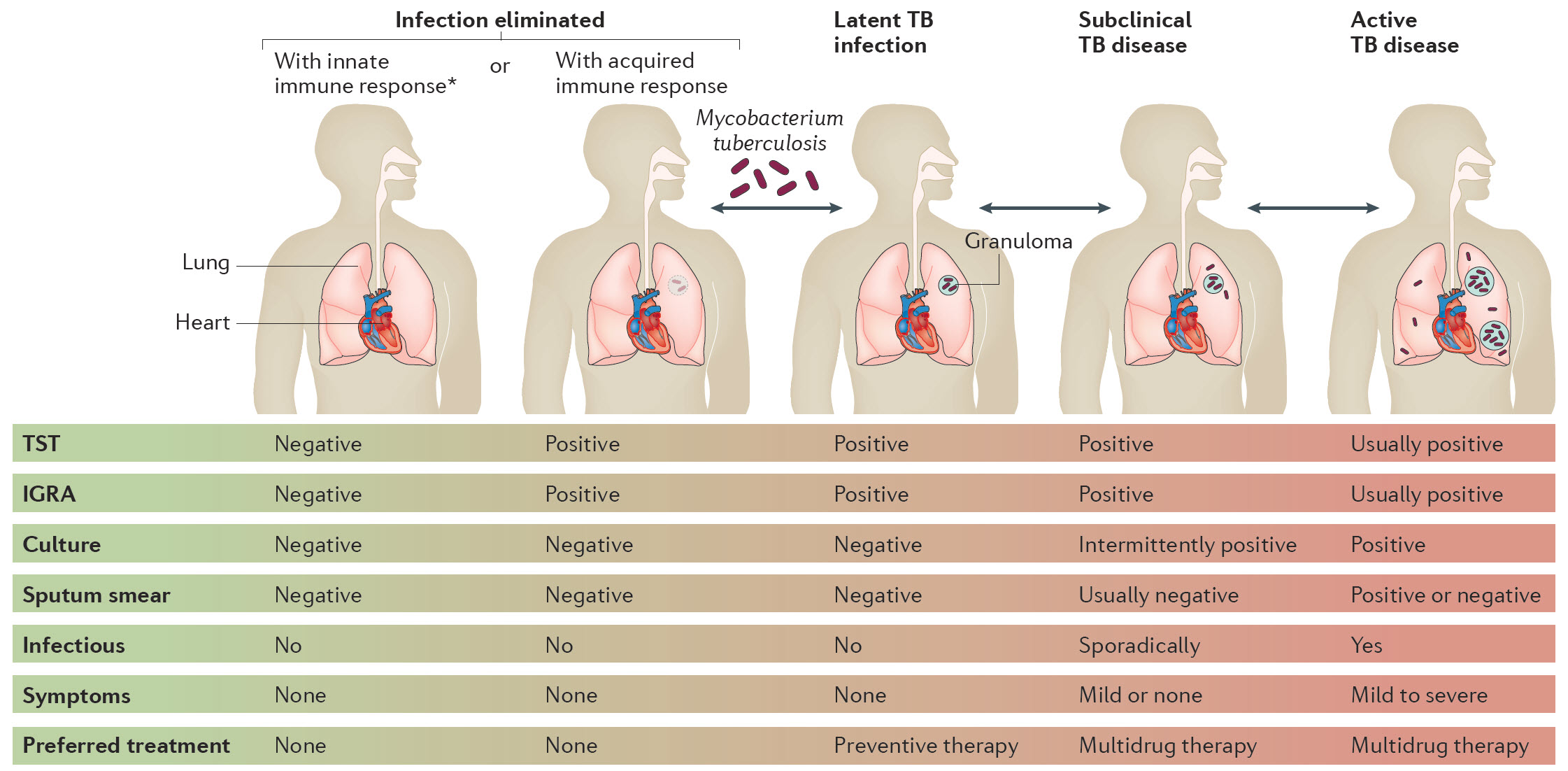
As shown in the graphic from our Primer, exposure to M. tuberculosis can result in the elimination of the pathogen, either because of innate immune response, or acquired T-cell immunity. Individuals who have eliminated the infection via innate immune responses, or with acquired immune response but without retaining immune memory, can have negative tuberculin skin test (TST) or interferon-gamma release assay (IGRA) results. All of us have probably heard of the TB clinic nurse who has been exposed repeatedly, but has never converted her skin test.
Some individuals will eliminate the pathogen, but retain a strong memory T-cell response and will be positive on TST or IGRA. These individuals will not benefit from LTBI treatment (typically, isoniazid for 6-9 months). If the pathogen is not eliminated, bacteria persist in a quiescent or latent TB infection that can be detected using a positive TST or IGRA result; these tests elicit T cell responses to M. tuberculosis antigens. It is estimated that 25% of the world's population is latently infected. But only a small proportion will progress to active TB disease.
Patients with subclinical TB might not report symptoms, but will be culture-positive (but generally smear-negative because of the low bacillary load).
Patients with active pulmonary disease experience symptoms such as cough, fever and weight loss, and the diagnosis can be usually confirmed with smear, culture and molecular tests. But active TB disease itself is a spectrum - can range from extrapulmonary TB, to pulmonary TB that is smear-negative, pulmonary TB that is smear-positive, and disseminated, severe disease.
Individuals with subclinical or active TB disease should receive one of the recommended treatment regimens for active TB disease, which consist of an intensive phase with four drugs, followed by a longer continuation phase with two drugs. Thus, the preferred treatment varies, depending on the stage in the 'spectrum' of TB.
One of the biggest challenges in TB is to understand why exactly some individuals successfully clear M. tuberculosis or maintain it as latent TB, while others progress to active and more severe forms of the disease (and even die). If we can crack this puzzle, it should help us develop better vaccines and host-directed therapies.



Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in