Why universal models of brain health will fail
Published in Social Sciences, Neuroscience, and Public Health

Current models of brain health are at a critical juncture. From omics to neuroscience, cognition, and brain diseases, we have tried to use universal models based on a limited subset of data to predict outcomes in extended global settings. This approach is inherently appealing; we desire a single set of risk factors in a hierarchical order to predict and promote healthy aging widely. We aim for a core cause of dementia to develop a universal treatment, potentially even a cure, addressing this complex disease. We expect clear and differentiated factors impacting brain diseases based on models with single and linear causes, linking specific deficits to particular conditions and core mechanisms. This attractive idea suggests that simple approaches can address complex settings.
However, brain health, aging, and dementia are not only complex but also heterogeneous, diffuse, and importantly, non-monolithic. For any statistical model, be it a simple ANOVA or a complex deep learning algorithm with multiple layers and efficient optimizers, the robustness of the models depends on data distribution. When data is heterogeneous, robust predictions in new data can be developed by incorporating data augmentation, heterogeneity-robust techniques, multicollinearity assessment, or performing data partition and cross-validation. However, models generally lose robustness as multimodal heterogeneity increases, leading to misclassification and non-replication. When data comes from diverse populations, where the heterogeneity is also multimodal, we face a more significant problem that cannot be solved merely by correcting algorithmic biases. Multimodal diversity (genetic, environmental, and lifestyle) strongly impacts brain health. In such cases, the generalization of predictive models fails, even when incorporating tools to handle data heterogeneity. The only way to obtain robust models is to acquire and include as much diversity as possible. This requires integrating multimodal heterogeneous data, including populations with different genetics, epigenetics, exposomes, and individual trajectories. In addition to incorporating multimodal diversity, more synergistic, whole-body-based, multi-pathway theoretical models are required. Yet, even then, the solution will not be a universal model generalized to all populations but tailored, personalized models. The future of global brain health lies in locally tailored and individually customized approaches.
Latin America is among the most diverse populations regarding genetic x environmental interactions, structural inequalities, complex exposomes, and variability in individual lifestyles and risk factors. In a recent study in Nature Aging, we conducted a meta-analysis and scoping review to assess risk factors for cognition and functional ability in aging populations across Latin America. We analyzed 38 reports from an initial pool of 455, with 146,000 participants. The results showed significant but highly heterogeneous effects on cognition (OR = 1.20, P = 0.03, I² = 92.1%) and functional ability (OR = 1.20, P = 0.01, I² = 93.1%, Fig. 1).
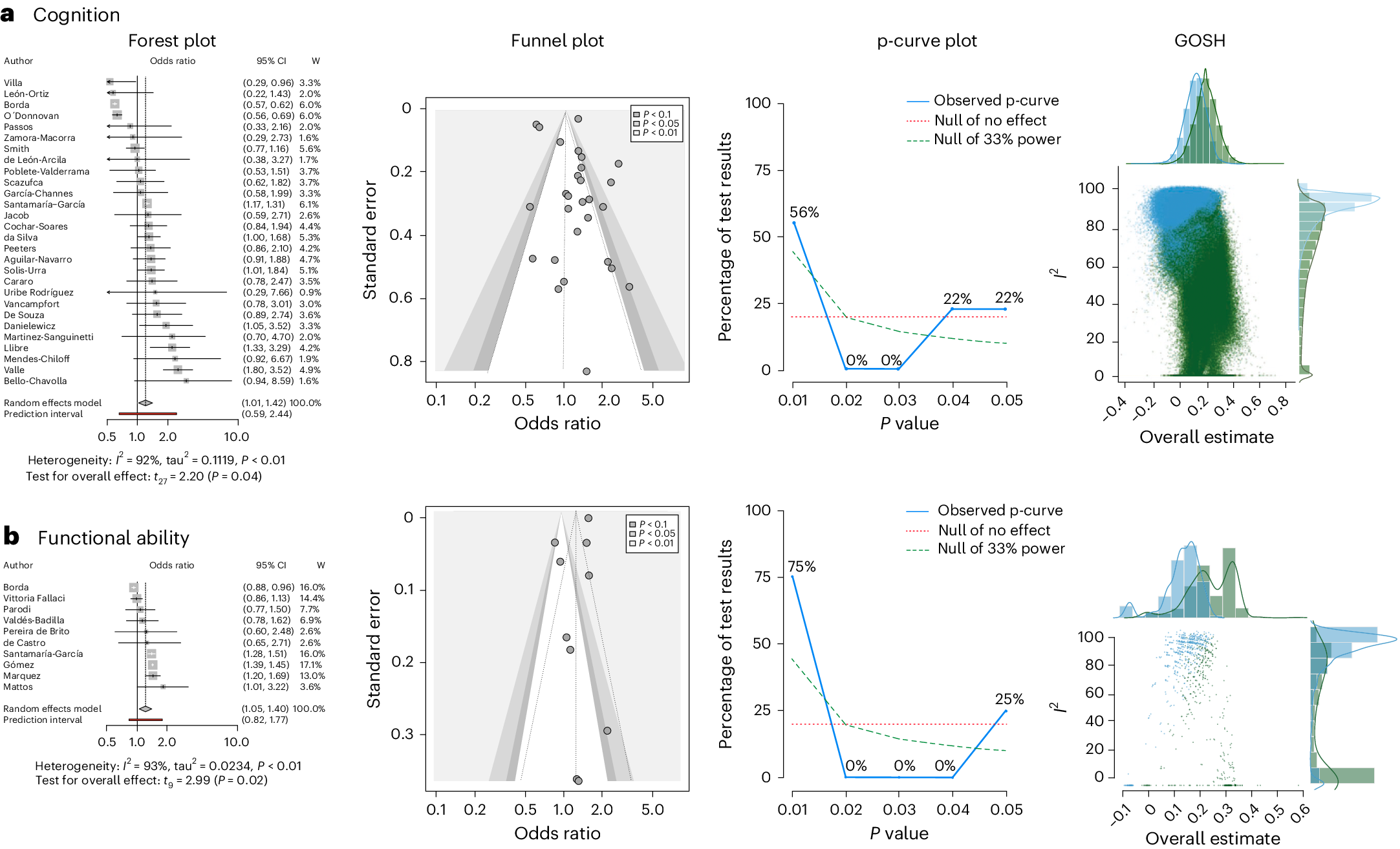
Fig. 1: Meta-analysis across all risk factors for cognition and functional ability.a, Cognition. Forest plot shows k studies in random effects model (first author, OR, CI and weights). The random effects model results (cognition: k = 28, n = 102,064, OR = 1.2006, P = 0.0363, CI = (1.0127, 1.4234); functional ability: k = 10, n = 99,428, OR = 1.2088, P = 0.0153, CI = (1.0470, 1.3956)) are reported with Knapp–Hartung correction for false discovery rate, the prediction interval and heterogeneity values (I2 and tau2). W, weights. b, Functional ability. Forest plot shows k studies in random effects model (first author, OR, CI and weights). The random effects model results (functional ability: k = 10, n = 99,428, OR = 1.2088, P = 0.0153, CI = (1.0470, 1.3956)) are reported with Knapp–Hartung correction for false discovery rate, the prediction interval and heterogeneity values (I2 and tau2). For a and b, contour-enhanced funnel plot shows effect sizes, standard errors and significance; p-curve analysis shows the accumulation of P values over the significant studies (observed p-curve), the no-effect curve and 33% power curve; and the GOSH shows distribution for all 2k−1 possible study combinations (1 million randomly selected models when 2k−1 > 106) in blue and leaving out the most negatively influential study in green.
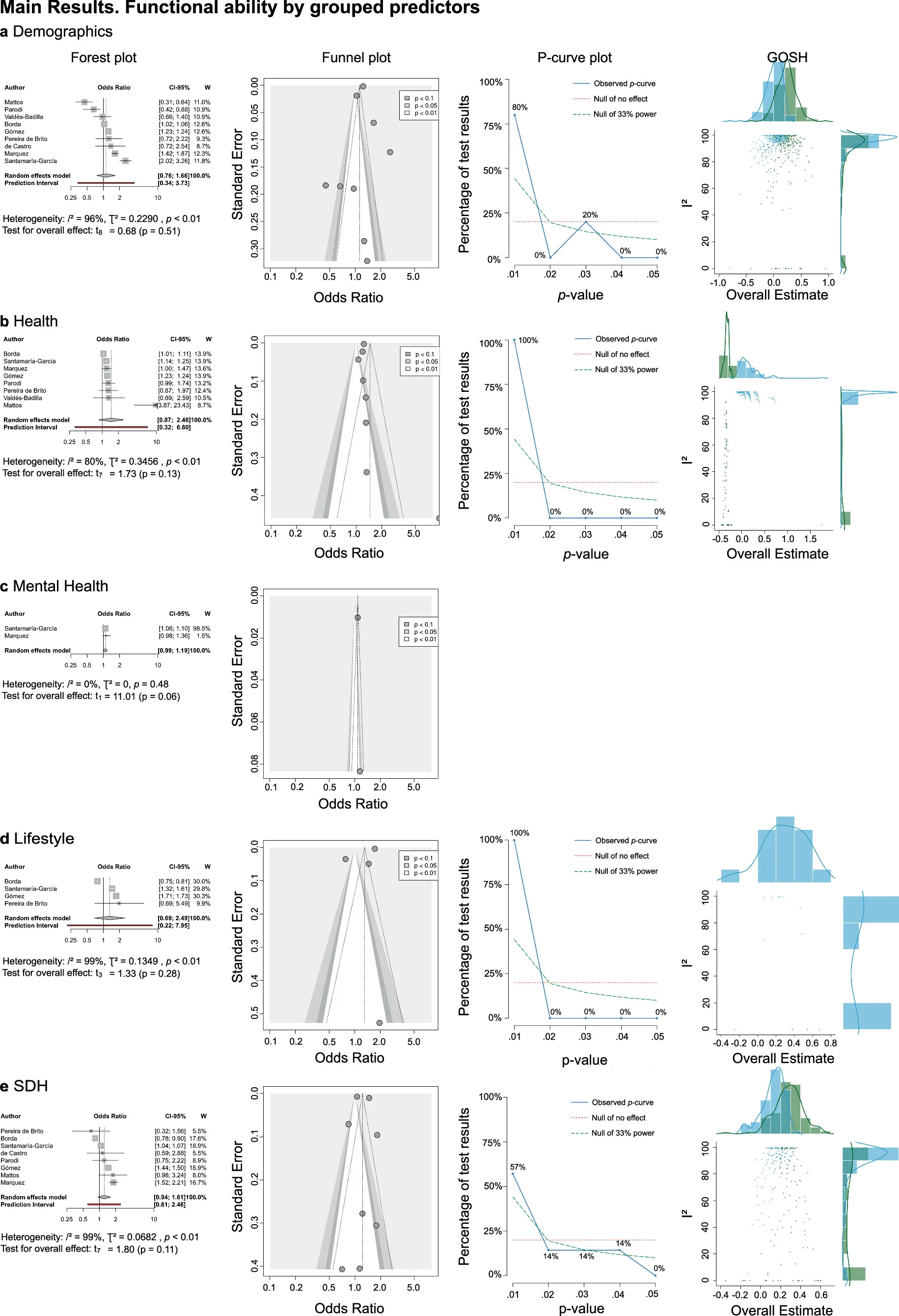
The effects of specific factors on healthy aging were less robust. Demographics significantly influenced cognition but showed substantial heterogeneity and publication bias (Fig. 2). The evidence for functional ability was weaker (Fig. 3), though an underlying actual effect existed. Health status was associated with cognition and functional ability but had high heterogeneity. Mental health significantly impacted cognition, with notable heterogeneity and potential publication bias, while effects on functional ability were non-significant. Social determinants of health (SDH) analyses mainly were non-significant, but p-curve analyses indicated an underlying minor impact. Conservatively ranking effects by confidence interval (CI) without outliers, demographics had the most substantial influence, followed by mental health and health status, with lifestyle and SDH being non-significant, contradicting previous reports.
%2016.00.19.png)
Each panel illustrates the major effects for each factor analyzed: panel a focuses on demographics; panel b on health; panel c on mental health; panel d on lifestyle; and panel e on Social Determinants of Health (SDH). The forest plot shows -k studies using the random effects model (first author, odds ratio, confidence interval, and weights). The random effects model results (Demographics: k = 15, n = 66634, OR = 1.5098, p-value = 0.0023, CI = [1.1905; 1.9147]; Health: k = 16, n = 67736, OR = 1.2856, p-value = 0.0397, CI = [1.0136; 1.6305]; Mental health symptoms: k = 16, n = 38679, OR = 1.6803, p-value = 0.0084, CI = [1.1848; 2.3830]; Lifestyle: k = 13, n = 89457, OR = 1.04, p-value = 0.7747, CI = [0.7765; 1.3930]; SDH: k = 15, n = 68250, OR = 0.9994, p-value = 0.998, CI = [0.6110; 1.6348]) are reported with Knapp-Hartung correction for false discovery rate, the prediction interval, and heterogeneity values (I², tau²). Contour-enhanced funnel plot showing effect sizes, standard errors, and significance. P-curve analysis, showing the accumulation of p-values over the significant studies (observed p-curve), the no-effect curve and 33% power curve. GOSH (Graphic Display of Heterogeneity) shows the distribution for all 2k-1 possible study combinations (1 million randomly selected models when 2k-1 > 106) in blue and leaving out the most negatively influential study in green.
The lack of consistent measures for SDH across studies and the inherent heterogeneity within Latin American countries might diminish the perceived importance of SDH. Classical approaches assume a similar profile of social adversity across the Global South, diminishing the understanding of the impact of region-specific factors on healthy aging. The prediction of functional ability was weaker than cognition, likely due to fewer studies and less direct assessment methods. Methodological issues like outliers, inter-country differences, and publication bias influenced the results. The study underscored the failure of universal models from the United States and Europe. It highlighted the need for more diverse, region-specific data to understand and promote healthy aging in Latin America accurately.
Each panel illustrates the major effects for each factor analyzed: panel a focuses on demographics; panel b on health; panel c on mental health; panel d on lifestyle; and panel e on Social Determinants of Health (SDH). The forest plot shows k studies using the random effects model (first author, odds ratio, confidence interval, and weights). Information on the P-curve and GOSH plot was not displayed in panel c due to a reduced number of studies available for conducting specific analyses. The random effects model results (Demographics: k = 9, n = 99120, OR = 1.1232, p-value = 0.5132, CI = [0.7593; 1.6613]; Health: k = 8, n = 98992, OR = 1.4634, p-value = 0.1264, CI = [0.8708; 2.4595]; Mental health symptoms: k = 2, n = 49257, OR = 1.083, p-value = 0.0577, CI = [0.9878; 1.874]; Lifestyle: k = 4, n = 80130, OR = 1.3086, p-value = 0.2756, CI = [0.6875; 2.4906]; SDH: k = 8, n = 98793, OR = 1.2273, p-value = 0.1144, CI = [0.9382; 1.6055]) are reported with Knapp-Hartung correction for false discovery rate, the prediction interval, and heterogeneity values (I², tau²). Contour-enhanced funnel plot showing effect sizes, standard errors, and significance. P-curve analysis, showing the accumulation of p-values over the significant studies (observed p-curve), the no-effect curve, and the 33% power curve. GOSH (Graphic Display of Heterogeneity) shows the distribution for all 2k-1 possible study combinations (1 million randomly selected models when 2k-1 > 106) in blue and leaving out the most negatively influential study in green. Blank panels indicate that P-Curves and GOSH cannot be estimated due to insufficient studies.
To translate scientific advances into real-world models impacting people's lives, we need to develop more robust science incorporating multimodal diversity, which is not just a moral imperative. This is a scientific one. Excluding exceptions and shortcuts, successful global brain health science based on data from a minority of the world will not be scalable to global settings. It is time to evolve into more realistic and robust models of brain health and reformulate new theoretical models to understand diversity and complexity.
Follow the Topic
-
Nature Aging

This journal’s mission is to provide a unique multidisciplinary, unifying and highly visible publishing platform for the aging-research community, with studies that cover the biology of aging and longevity.
Your space to connect: The Psychedelics Hub
A new Communities’ space to connect, collaborate, and explore research on Psychotherapy, Clinical Psychology, and Neuroscience!
Continue reading announcement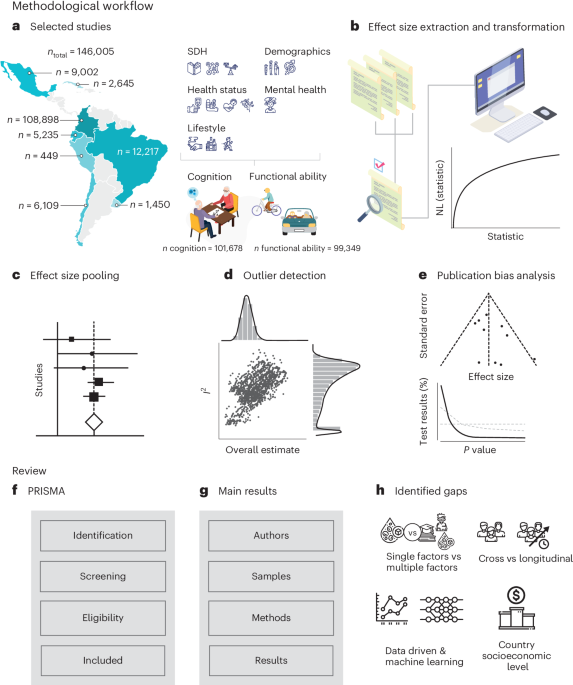



Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in