World AMR Awareness Week 2025 – Break the Chain of Resistance: Insights from the BMC Series articles
Published in Microbiology and Pharmacy & Pharmacology

Antimicrobial resistance (AMR) is a growing global health threat with serious consequences for treatment success and healthcare costs. From routine surgeries and chemotherapy to safe childbirth and intensive care, antimicrobials underpin countless lifesaving interventions—but their effectiveness is fading. Misuse and overuse accelerate resistance, allowing bacteria to outpace drug development. The result is a slow-moving pandemic that could turn once-treatable infections deadly, especially for vulnerable patients. Its impact ripples across health systems: longer hospital stays, higher costs, and fewer treatment options. Yet this complexity also offers opportunities for action.
This blog delves into research spanning cancer wards fighting superbugs to the role of self-medication in driving resistance, while emphasizing that solutions exist: antimicrobial stewardship can optimize prescribing, vaccines can prevent infections, diagnostics enable targeted treatment, education can transform behaviors, and policy can align incentives for responsible use.
AMR in cancer care: a high‑stakes vulnerability
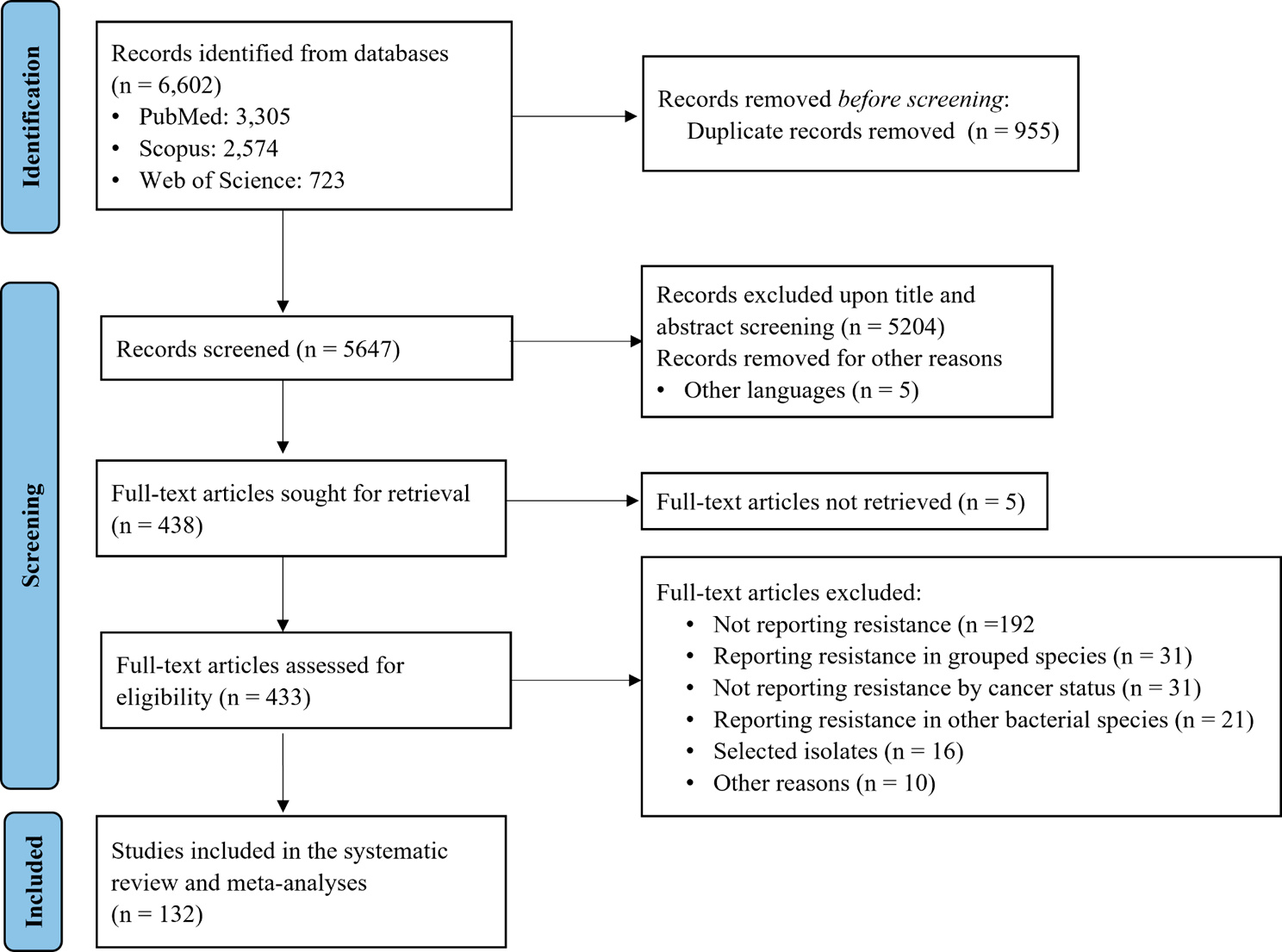
BMC Infectious Diseases- “Antimicrobial resistance of bacterial pathogens isolated from cancer patients: a systematic review and meta‑analysis”
Cancer patients face a heightened risk of antibiotic-resistant infections due to frequent invasive procedures, indwelling devices, and broad-spectrum antibiotic use. Their weakened immunity makes treatment failures potentially life-threatening, underscoring the need for targeted strategies in oncology care.
This systematic review and meta-analysis provides the first global assessment of AMR prevalence among bacterial pathogens in cancer patients. Drawing from 132 studies published between 2000 and 2024, the review found hematologic cancer patients—36.4% of cases—most affected, reflecting their intensive chemotherapy and prolonged hospital stays.

The findings reveal alarming resistance patterns among major pathogens, including E. coli, Klebsiella pneumoniae, Staphylococcus aureus, Acinetobacter baumannii, Pseudomonas aeruginosa, Enterococcus faecium, and Enterobacter species. Klebsiella pneumoniae showed penicillin resistance of nearly 99%, while Acinetobacter baumannii exhibited multidrug resistance across cephalosporins (84%), carbapenems (83%), and fluoroquinolones (80%). These ESKAPE pathogens dominate hospital-acquired infections and evade multiple antibiotic classes.
The implications are severe: limited treatment options force reliance on costly, toxic last-resort drugs, compromising outcomes and accelerating the AMR crisis. The review calls for urgent action—robust infection prevention, antimicrobial stewardship, global surveillance, and investment in new antibiotics and alternative therapies.
Preventing resistant Salmonella through vaccination and hygiene
BMC Infectious Diseases “Combatting Salmonella: a focus on antimicrobial resistance and the need for effective vaccination”
Salmonella infections remain a major global public health challenge, driven by their zoonotic nature, increasing antimicrobial resistance, and significant morbidity and mortality. These infections are transmitted primarily through contaminated food and water, making them particularly prevalent in regions with inadequate sanitation and food safety standards. The growing resistance of Salmonella strains to multiple antibiotics has compounded the problem, limiting treatment options and increasing the risk of severe outcomes.
This systematic review focused on studies addressing the epidemiology of Salmonella, vaccine development, and strategies for controlling infections. The findings reveal that Salmonella infections burden is disproportionately high in low- and middle-income countries, where poor sanitation, limited access to clean water, and inadequate food safety practices facilitate transmission. Among the numerous serovars of Salmonella, Enteritidis and Typhimurium are the most commonly associated with human infections. These strains have shown a troubling rise in multidrug resistance (MDR), largely attributed to the overuse and misuse of antibiotics in both human medicine and livestock production.
Despite progress in vaccine research, a universal Salmonella vaccine remains elusive. Current candidates—live-attenuated, killed, recombinant, subunit, and conjugate—face challenges of efficacy, cost, and accessibility. The diversity of serovars and complex immune responses further complicate development.
Addressing this dual threat requires a multifaceted approach: improved sanitation, prudent antibiotic use, accelerated vaccine development, stronger surveillance, and global collaboration. Without urgent action, Salmonella infections and AMR will continue to undermine public health security.
Aztreonam-Avibactam: A Promising Option Against Resistant Bloodstream Infections
BMC Infectious Diseases - “Antimicrobial susceptibility of Enterobacterales causing bloodstream infection in U.S. medical centres: comparison of aztreonam–avibactam with β‑lactams active against CRE”
Bloodstream infections (BSIs) are among the most dangerous bacterial infections, and when treatment is delayed, outcomes can be dire. The challenge has grown as certain bacteria—Enterobacterales—develop powerful resistance mechanisms like metallo-β-lactamases (MBLs) and OXA-48–like carbapenemases. These enzymes render many standard antibiotics ineffective, leaving clinicians with few options.
Aztreonam-avibactam, a novel therapy currently in development. Unlike existing drugs, it targets Gram-negative bacteria, including those producing MBLs—organisms that are notoriously hard to treat.
A recent study across 72 U.S. hospitals (2020–2022) tested 4,802 Enterobacterales isolates to compare aztreonam-avibactam with other advanced antibiotic combinations. The results were remarkable, 98% of carbapenem-resistant Enterobacterales (CRE) were inhibited by aztreonam-avibactam. It retained activity even when other drugs failed, including against MBL and OXA-48 producers. Only two isolates showed resistance beyond the susceptibility threshold.
Current therapies like ceftazidime-avibactam and meropenem-vaborbactam work well against KPC-type resistance but falter against MBLs. Aztreonam-avibactam bridges that gap, offering a much-needed option for critically ill patients.
In conclusion, as antimicrobial resistance rises globally, aztreonam-avibactam could become a cornerstone in treating life-threatening BSIs. Its ability to overcome resistance mechanisms that defeat other drugs makes it a promising candidate for future clinical practice.
Self‑medication fuels resistance in the community
BMC Public Health- “Prevalence and predictors of self‑medication with antibiotics among adults in Santo Domingo and the National District, Dominican Republic”
Antibiotic self-medication is a growing public health concern that significantly contributes to the global challenge of antimicrobial resistance (AMR). This issue is particularly acute in low- and middle-income countries, where regulatory oversight of antibiotic dispensing is often inadequate. While antibiotic stewardship programs have largely focused on healthcare facilities, community-level practices remain poorly regulated, allowing individuals to access antibiotics without prescriptions. This unmonitored use accelerates resistance, undermining the effectiveness of essential medicines and posing a serious threat to public health.

A recent cross-sectional study conducted in October 2024 sought to assess the prevalence of antibiotic self-medication among adults in Santo Domingo and the National District of the Dominican Republic, as well as identify sociodemographic factors associated with this behavior. The study surveyed 687 participants, revealing that 14.6 percent reported self-medicating with antibiotics within the previous 12 months. Amoxicillin emerged as the most commonly used antibiotic, accounting for 69 percent of reported cases, and nearly all respondents (98 percent) obtained these drugs from pharmacies without prescriptions. Convenience was cited as the primary motivation for self-medication by 56 percent of participants, reflecting a preference for quick and accessible solutions over formal medical consultations. Common symptoms prompting antibiotic use included sore throat (55 percent) and nasal congestion (23 percent), conditions often caused by viral infections for which antibiotics are ineffective.
The findings suggest that financial constraints and limited access to healthcare services drive self-medication behaviors, perpetuating inappropriate antibiotic use and resistance. The study underscores the urgent need for targeted interventions to curb antibiotic misuse at the community level. Public awareness campaigns should emphasize the dangers of self-medication and the importance of seeking professional care for common illnesses. Pharmacies, as primary points of access, must play a central role in promoting responsible antibiotic use through education and compliance with prescription-only regulations. Strengthening enforcement of these regulations in the Dominican Republic is critical to reducing unregulated antibiotic sales and mitigating the spread of AMR.
Stewardship starts in the classroom
BMC Medical Education - “Antimicrobial stewardship competencies in undergraduate dental education: a multicentre cross‑sectional study of clinical dental students in Southern Nigeria”
Antimicrobial stewardship (AMS) is a cornerstone of global health strategies aimed at promoting rational antimicrobial use to combat the escalating threat of antimicrobial resistance (AMR) and improve patient outcomes. While AMS initiatives have traditionally focused on medical practice, dental practitioners also play a significant role in antibiotic prescribing, particularly in outpatient care.
In this study a multicentre cross-sectional survey was conducted among 160 clinical dental students from three universities in southern Nigeria. The findings revealed a generally positive baseline knowledge and attitude toward AMS among the students. However, notable demographic variations were observed. Male students, younger participants, Muslims, and those from minority ethnic groups demonstrated higher AMS competencies compared to their counterparts. A strong positive correlation was identified between knowledge and attitude scores, suggesting that improved understanding of AMS principles translates into better attitudes toward stewardship practices.
Further analysis revealed that gender and marital status were significantly associated with knowledge scores, while marital status also influenced attitudes toward AMS. Institutional differences were evident, with students from the University of Nigeria recording lower AMS knowledge scores compared to those from other participating schools. These disparities highlight gaps in the uniformity of AMS education across dental institutions in the region.
The study concludes that while clinical dental students in southern Nigeria exhibit adequate baseline knowledge and attitudes toward AMS, demographic and institutional differences underscore the need for targeted educational interventions. This research emphasizes the importance of incorporating comprehensive AMS training into dental education. By equipping future dental practitioners with the necessary knowledge and attitudes, healthcare systems can reduce inappropriate antibiotic prescribing and play a pivotal role in combating antimicrobial resistance—a challenge that continues to threaten global health security.


Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in