World Hepatitis Day 2017 |One year into the WHO viral hepatitis strategy: are we all doing our part?
Published in Microbiology

It has been a little more than a year since the World Health Organization (WHO) introduced its first-ever Global Health Sector Strategy on Viral Hepatitis.
Some people working in the viral hepatitis field seem to think of the strategy as something that only matters to distant technocrats. Other people don’t think about it at all.
This is actually a big problem. Why? Because adapting key elements of the global strategy into national viral hepatitis strategies around the world is our best bet for eliminating this group of diseases. In order to defeat viral hepatitis, governments must establish a complex array of public health interventions targeting diverse populations. They simply cannot afford to waste time and money re-learning things that already are known about what does and does not work.
The WHO strategy provides a wealth of evidence-informed guidance regarding how governments should integrate awareness, prevention and treatment into viral hepatitis programmes that need to successfully balance many competing priorities.
So why should you care about the strategy if you do not work for WHO or a national or regional ministry of health? Because we need everyone who is contributing to the drive to eliminate viral hepatitis – be that through research, health services, personal advocacy or some other means – to raise their voices when government efforts are misguided.
The ideal public health responses will not just happen on their own. The strategy provides a checklist for what stakeholders at all levels should be demanding from their governments, and also points to contributions that all of us can make to informed decision-making.
Consider, for example, a key organising framework presented in the strategy: the continuum of viral hepatitis services and retention cascade (Fig. 1).
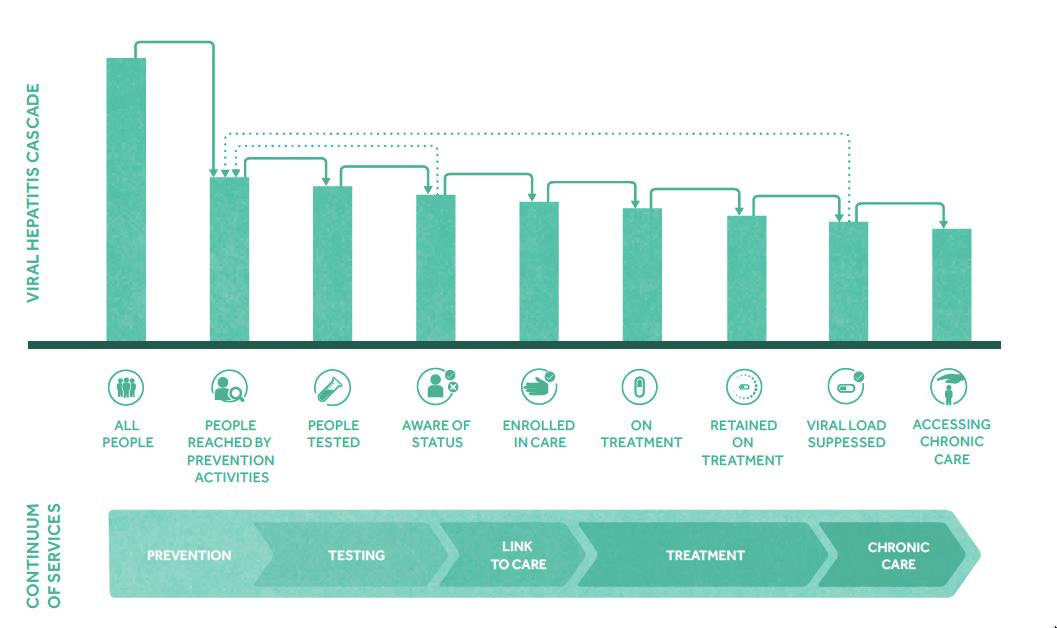
Fig. 1. WHO’s continuum of viral hepatitis services and retention cascade. Reprinted from the Global Health Sector Strategy on Viral Hepatitis 2016-2021, p.19, World Health Organization, copyright 2016.
The strategy advises governments to integrate this continuum into their national monitoring frameworks so that they will be able to identify key points at which opportunities to treat and cure individuals are lost – for example, when people who have received positive hepatitis test results are not linked to care, or when people who are enrolled in care do not initiate treatment.
As discussed in a Comment co-authored by the authors of this blog, many national governments currently are unable to report accurately or comprehensively on the numbers of people progressing through the hepatitis B and hepatitis C cascades in their countries. This means that they also lack the information that is required for appropriate priority-setting at the national and subnational levels.
What might the implications of this lack of data be for you, in terms of your own viral hepatitis work? And what can you do to encourage decision-makers to give more attention to this issue?
Besides directly engaging with influential stakeholders, consider integrating the continuum of care framework into any reporting in which you are involved. By consistently demonstrating the utility of the continuum of care for tracking progress against viral hepatitis within individual clinics, hospitals, municipalities and community-based programmes, organisations outside of government can contribute to establishing the continuum of care as the universal reporting norm.
It’s too easy to dismiss far-reaching global policy documents as empty rhetoric. In order to halt suffering and death from viral hepatitis, we need to take stock of the tools that we have available to us and put them to use. Consistently implementing well-reasoned strategies and evidence-based interventions is the first step.
Jeffrey V. Lazarus and Kelly Safreed-Harmon



Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in