Donation of Unused Surplus Frozen Eggs by former Elective Egg Freezing (EEF) Patients - Counseling of Prospective Donors
The majority of women who undergo elective egg freezing (EEF) do not eventually utilize their frozen eggs, which thus represent a promising source of donor eggs.
Published in Pharmacy & Pharmacology and Philosophy & Religion
Like
Be the first to like this
Please refer to the following academic journal article:
Counseling Elective Egg Freezing Patients Considering Donation of Unused Surplus Frozen Eggs for Fertility Treatment
Here is a longer and more detailed video presentation of this article:
A systematic, two-step counseling protocol for women who have undergone Elective Egg Freezing (EEF) and are considering donating their surplus frozen eggs is hereby proposed. EEF involves freezing eggs for non-medical or social reasons, such as delaying motherhood to pursue educational and career opportunities, difficulty finding a spouse/partner, or fulfilling personal lifestyle aspirations.
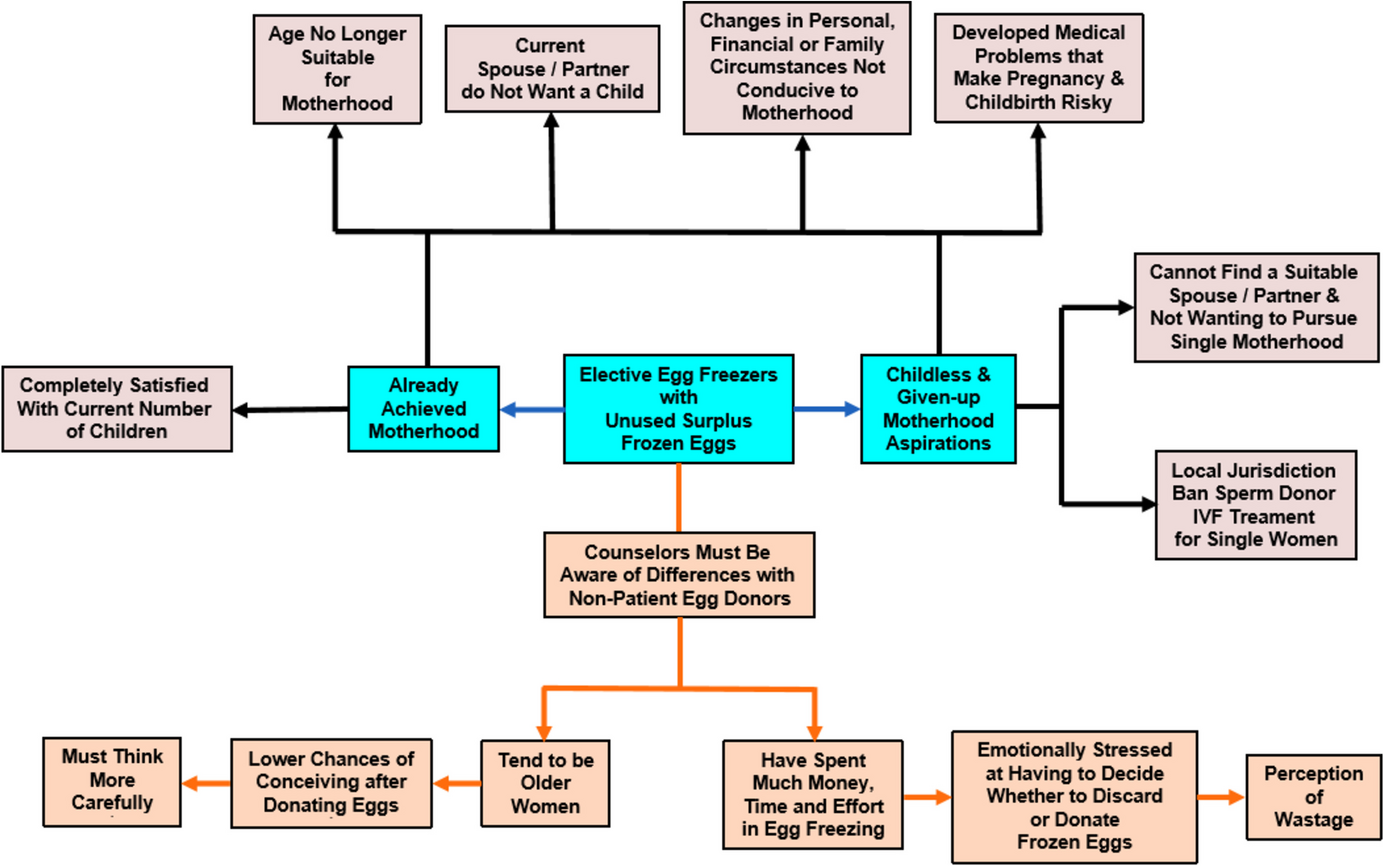
The core issue addressed is that the majority of women who undergo EEF do not eventually utilize their frozen eggs (approximately 80%). This non-utilization occurs for various reasons, including successful natural conception post-procedure, advanced age making motherhood impractical, or inability to find a suitable partner, sometimes influenced by sociocultural factors like religion preventing single motherhood via donor sperm. The resulting accumulated surplus represents a promising source of donation for infertile women with depleted ovarian reserves undergoing in vitro fertilization (IVF) treatment. Roughly 25–30% of former EEF patients choose to donate their surplus eggs, suggesting 20–25% of all frozen eggs may eventually be donated.
Ethical Imperative for Counseling
Rigorous, systematic, and comprehensive professional counseling is essential because the decision to donate unused frozen eggs involves complex decision-making and careful deliberations. Since most EEF patients will not use their frozen eggs, they should be informed before the EEF procedure begins that they will eventually need to make complex decisions regarding disposal. The process of deciding what to do with unused eggs is often emotionally draining and heart-wrenching, particularly for those whose dream of motherhood failed due to reasons like advanced age or inability to find a partner. Counseling is crucial for providing accurate information and discussing all possible options, thereby helping patients overcome challenges such as decision fatigue and a lack of information.
While most jurisdictions require psychological counseling for prospective egg donors, a major deficiency is the lack of standardized, systematic counseling protocols, which often leaves the issues discussed and the counseling style dependent on the counselor's idiosyncrasies. Furthermore, counseling has traditionally focused on conventional non-patient donors, neglecting the unique circumstances of former EEF patients.
Unique Circumstances of EEF Donors
EEF donors differ significantly from conventional egg donors. Firstly, EEF donors tend to be much older when they consider donating their surplus eggs. This older age drastically reduces their chances of conception should they later regret the donation, meaning there is "no turning back their biological clock" once the donation is complete. Conventional donors, being younger, retain many more years of fertility. Secondly, EEF donors have invested substantial money, time, and effort into the egg freezing procedure and have paid expensive cryostorage fees for several years. Consequently, they are often under emotional stress and perceive the decision on disposal as a "waste of their hard-earned money," unlike conventional donors whose medical fees are usually fully covered by recipients.
Basic Principles and Autonomy
Crucially, counseling must be neutral and should not encourage donation or focus on the needs of infertile patients. The potential for others to benefit from the donation is irrelevant to the patient’s decision and could bias the counselor. Counseling must ensure autonomous decision-making without undue influence. A comprehensive protocol must discuss all possible disposition options, including destruction, donation for research, or teaching/training, besides donation for fertility treatment. A significant conflict of interest exists if doctors who performed the initial EEF procedure solicit donations, as they stand to earn additional medical fees from the donation procedure. Patients must also be given adequate time to finalize their decision due to the complexity and emotional stress involved.
The Two-Step Systematic Counseling Protocol
The proposed two-step systematic protocol is designed to facilitate informed decision-making:
STEP 1: Verify and Ensure Non-Use Intentions The first step is critical: fertility counselors must verify and ensure prospective EEF donors genuinely and sincerely have no future desire to use their frozen eggs to conceive a child for themselves. This verification is key to avoiding future decision regret. EEF donors fall into two categories: those who have achieved motherhood and those who remain childless. Childless EEF patients may cite factors such as inability to find a suitable partner, religious/sociocultural reasons for avoiding single motherhood with donor sperm, or local laws banning certain IVF options. Factors common to both groups include age being unsuitable for motherhood, current partner disapproval, or adverse financial/medical circumstances.
STEP 2: Discuss Motivating and Dissuading Factors and Present Other Options
The second step involves a comprehensive discussion of motivating and dissuading factors related to donation:
• Motivating Factors: Common motivations include goodwill to help infertile patients and avoiding the wastage of eggs, given the money, time, and effort invested. EEF patients who have achieved motherhood are often motivated by a sense of reciprocity and a desire to share the joy of motherhood. However, ethically problematic motivations include the undue inducement of partial or full reimbursement of medical fees, which compromises autonomous decision-making. Contentious market forces may also influence reimbursement based on donor characteristics like prestigious degrees or physical attributes (e.g., height, complexion), potentially sparking racial discrimination accusations if ethnic minority women cannot receive reimbursement due to a lack of demand. For the rare childless donor, a hypothesized motivation is preserving their genetic lineage.
• Dissuading Factors: Key apprehensions include the fear of accidental incest between natural and unknown donor-conceived offspring, sometimes related to "Genetic Sexual Attraction". Another major concern is the apprehension of unexpected future contact with unknown donor-conceived offspring due to the abolition of donor anonymity in some jurisdictions or the widespread use of consumer DNA testing and online genealogy websites. Other dissuading factors involve potential future regret, lack of benefits from altruistic donation, spousal/partner disapproval, hassles of required testing, or religious/cultural prohibitions. Religious factors, such as Shariah injunctions prohibiting Sunni Muslims from gamete donation due to "muddling of lineage," or Confucian emphasis on bloodline integrity, require cultural sensitivity from counselors. Childless EEF patients may also be discouraged by disappointment over their failed motherhood aspirations.
Regulatory Safeguards and Information Disclosure
The following additional safeguards to protect the rights of EEF donors and recipients are recommended:
1. Donor Protections: EEF donors must be mandated to undergo screening for common genetic diseases (like cystic fibrosis or sickle-cell disease) and infectious diseases before donation, as they may not have been screened initially. To prevent future decision regret, older EEF patients (over 37 years old) should be required to have at least one child before donating. Spousal/partner involvement in counseling is recommended, especially given the risk of accidental incest. Monetary reimbursement should preferably be disallowed or, if permitted, ensured as a fixed, equal sum regardless of race, educational level, or physical appearance to prevent discrimination and undue inducement. Donors must be allowed to withdraw consent at any time before egg utilization. A hiatus of at least one week between counseling and signing consent forms is advised. Furthermore, doctors who previously performed the EEF procedure should not solicit donations to avoid abusing the doctor-patient fiduciary relationship.
2. Recipient Information: Recipient patients must be informed that IVF success rates are significantly and consistently lower with frozen donor eggs compared to fresh donor eggs, especially since EEF donors are often older when they freeze their eggs, resulting in lower egg quality. Recipients should also be informed of the number and sex of children the donor already has, which aids in preventing accidental incest among offspring. To ensure distributive justice, fertility clinics should not control egg allocation; this prerogative should belong to a government agency based on need and a waiting list. Clinics should be banned from the unethical practice of dividing a single EEF donor's cohort of frozen eggs among multiple recipients to maximize medical fees.
3. Anonymity and Matching: The article suggests that donor anonymity should preferably be abolished, allowing donor-conceived offspring access to the donor's personal information upon reaching the age of majority (e.g., 21 years old), which is crucial for identity and self-esteem development. Additionally, strict matching of prospective recipients and donors based on ethnicity and physical characteristics (such as height, skin complexion, and hair color) should be enforced to prevent discrimination against donors based on physical appearance and ensure the donor-conceived offspring look similar to the recipient patient.
Follow the Topic
Assisted Reproductive Techniques
Life Sciences > Health Sciences > Clinical Medicine > Therapeutics > Assisted Reproductive Techniques
Bioethics
Humanities and Social Sciences > Philosophy > Moral Philosophy and Applied Ethics > Bioethics
Scholars at Risk
Research Communities > Scholars at Risk

Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in